Let’s Talk About The Current Opioid Crisis & Pain Prescription Crackdown
Recently there has been so much news about pandemics such as COVID 19, but nobody is talking about an epidemic that is causing more deaths than this global crisis. The Opioid Crisis is an epidemic is expanding on a global scale. In Australia, the rise in prescribing of pain medications, particularly opioids has increased signficantly. This is having has had devastating results, with the levels of harm and deaths due to opioid misuse rising exponentially.
In Australia, over three million people were prescribed 15.4 million opioid scripts in 2016–17. What is most concerning is that opioids now account for 62% of drug-induced deaths, with pharmaceutical opioids now more likely than heroin to be involved in opioid deaths and hospitalisations. In 2016–17 there were 5,112 emergency department presentations and 9,636 hospitalisations due to opioid poisoning, with three deaths per day attributed to opioid harm – higher than the road toll.(2)
The global crisis of opioid crisis is increasing and is very concerning. About 275 million people worldwide (5.6 per cent of the global population aged 15–64 years) used drugs at least once during 2016. There were an estimated 27 million people who suffered from opioid use disorders in 2016. Roughly 450,000 people died as a result of drug use in 2015. Of those deaths, about 118 thousands with opioid use disorders.
Overdose deaths contribute to between roughly a third and a half of all drug-related deaths, which are attributable in most cases to opioids. Lifetime prevalence of witnessed overdose among drug users is about 70%. There are effective treatments for opioid dependence yet less than 10% of people who need such treatment are receiving it. The inexpensive medication naloxone can completely reverse the effects of opioid overdose and prevent deaths due to opioid overdose.
Due to their pharmacological effects, opioids in high doses can cause respiratory depression and death.
In Australia today, unrelieved pain is a major issue. Up to 80 percent of people living with chronic pain are missing out on treatment that could improve their health and quality of life. Some of these people are dismissed and feel isolated and suffer constant pain, anxiety, depression and even attempt suicide. It is big issues that needs to be address.
Opioids and pain medications should never be regarded as the sole approach to people with chronic pain. They should be regarded as one component of a multimodality approach and management plan, and should only be used on a limited basis and monitored regularly so as not to develop and addiction.
A well-defined and well-structured multimodality management pain plan, set out be a qualified healthcare professional, is essential in improving pain outcomes, improving overall health and helping with the complications of withdrawal of pain medications and opioids.
In this video I talk about the current reforms here in Australia and the ongoing opioid crisis that needs urgent attention and people do need to be managed better on all levels.
Regards
Andrew Orr
-No Stone Left Unturned
-Master of Women’s Health Medicine
-Men and Women’s Health Advocate
-The Headache, Migraine and Pain Experts
References
- Deloitte Access Economics (2019), The cost of pain in Australia.
- Royal Australian College of General Practitioners (2018). Australian overdose deaths are increasing – and the demographics are changing. News GP. Access online here.
- WHO- Information sheet on opioid overdose (click here to access)
- Pain Australia (fact sheets)
Let’s Talk About Sex- How often, what’s normal & how to boost that libido
Sex is something that nearly every human on this planet gets to experience, and for each person, the experience of sex can be different. Many people have different perceptions on this important topic, so lets talk about sex, how often, what’s normal and how to boost that libido in those having issues.
As a healthcare practitioner who is a Master in Women’s Health Medicine and a Master of Reproductive medicine, I have to talk about the topic of sex on a daily basis. A lot of people come into my clinic (both men and women) with varying expectations and thoughts on what is normal, when concerning sex. Unfortunately a lot of people are way off the mark when it comes to a healthy sex life and what a healthy libido should be.
Libido is influenced by our health
If you do not have a healthy libido, there could be something wrong with your health. Yes, what you eat, think, do etc, all plays a part in your sexual appetite. But, we can all have differing libido’s and it is important to understand this and seek help if you are having issues. A healthy libido is a sign of a health body and healthy mind.
What defines a healthy sex life
The average healthy human being in a healthy relationship should be having sex at least 1-3 times per week, depending on age etc. I know a lot of you are lucky to be having sex 3 times per month.
What’s concerning about this is, some of these people are trying to have a baby and can’t understand why they aren’t falling pregnant. The answer is obvious, but, I’ll say it anyway, you have to have sex regularly to fall pregnant and it has to be at the right time. You need to be trying every day, or every second day of your cycle as we now know ovulation just doesn’t take place mid-cycle only.
Clinical research shows that more than 70% of people are ovulating before day 10 and after day 17 of their cycle. So if you are just trying it that small window of day 10-16, this could be the reason you aren’t falling. Btw, don’t stop having sex just because you are doing IVF. Sex (climax in particular) helps with implantation so stopping having sex is only hindering your chances of conception. I have talked about this is a previous post (click here to read)
We also now know that sperm also play a part in a health menstrual cycle as they help to trigger certain hormones to trigger ovulation and thus help with regulation of the menstrual cycle. It may explain why women using barrier methods of contraception have more issues with irregular cycles and menstrual issues. Not that we are promoting unsafe sex mind you. This is for couples in a healthy relationship. I have spoken about this is a previous post too (click here to read)
Why is climax/orgasm so important
Climax also stimulates blood flow into the uterus; helps trigger certain hormones and also helps with implantation. Climax also helps ones libido and it can even help in the treatment of depression.
We also hear the jokes about men and their ever-constant desire to have sex, but most of the time this is greatly exaggerated. In practice I am actually seeing that women are now the ones with the higher libidos and it is the men that are having all the problems. Stress is a big factor these days. We are also seeing many men with testosterone deficiency. Being overweight and unhealthy physically and mentally can be a factor also.
It has also been shown that regular sex, even if scheduled, actually helps with the libido and helps with the desire around wanting more sex.
Understanding differing libido’s
Men and women are different when it comes to libido and the desire around sex. Men need to understand that it can often take all day for a woman to arouse her desire around wanting sex. Men need to know that women need to be wooed, given playful thoughts, mind play and a place to feel safe to get her into the mood for sex. Guys, apparently helping out around the house also helps (hint, hint)
Intimacy is more than just sex
Remember sex is a healthy part of a relationship and a healthy libido shows good health. Sex is also a way of connecting with your partner and couples should find way to prioritise each other so that this connection happens regularly. It is also about intimacy and that sacred intimacy, which is on a whole other level to the physical act of just having sexual intercourse.
What affects a libido?
Many people do talk about having differing libido’s, or having trouble with libido, and it is important to understand what may be affecting ones sex drive.
So, what are some of the main things that effect libido?
- The Pill – First and foremost, the pill for women. Anything that decreases fertility can decrease your sexual desire. The pill also turns off certain receptors responsible for conception, which can then turn off the libido.
- Stress – Constant low grade, or high grade stress, is a big problem when it comes to loss of libido. It can cause impotence & erectile dysfunction in men and loss of libido and menopausal symptoms in women.
- Medications – Drugs such as anti-depressants, the pill, anti-inflammatories, and lots of other medications can ruin your sex life. They can also delay or stop orgasm. There are some that can improve it too. Not many!
- Alcohol and recreational drugs– This one is pretty self explanatory. We’ve all heard the saying ‘Fosters flop’ from drinking too much beer. Drugs such as marijuana, speed, and other illicit drugs can all impair libido
- Sexual Abuse– A history of sexual abuse can definitely affect the sex life. This needs to be dealt with by speaking to a counsellor, psychologist or sex therapist.
- Health Problems– Health problems such as Low Thyroid, Diabetes, being overweight, depression, eating disorders, can interfere with your libido and sex life.
- STD’s– Some STD’s are often undetected and cause pain and discomfort during sex, which leads to not wanting to have sex. Many of these can be cleared up with medication so that your sex life can return to normal. Some STD’s are there for life but can be controlled. STD’s such as herpes and HIV don’t have to stop your sex life.
- Gynaecological issues – Some gynaecological disease states such as Endometriosis and Adenomyosis can make sex painful and cause a lack of desire. Have a read of my article about painful sex. Women with PCOS can have low libido as a result of hormonal fluctuations and insulin resistance.
- Diet– This is a big one. If you eat the wrong foods the body will respond accordingly. Your sex life can be ruined by what you put in your mouth to sustain your body.
- Exercise– Over-exercising can stop you getting a period and cause fertility issues in both men and women. Reduce the exercise and the libido will respond accordingly. Exercise can also increase libido. It is about moderation.
Final Word
If you are having trouble with your libido there are many medical and natural products that have been shown to assist with low libido and help with a healthy sex life for both men and women. It is important that you talk to a qualified healthcare practitioner about issues to do with sex and libido. You need to see an expert who is trained to know issues that may be causing your particular issues. The can also give you dietary and lifestyle advice to help in this area too.
If you do need help with issues around sex and libido, please give my friendly staff and call and find out how I can assist you. I also have a great network of sex therapists, psychologists and medical specialists I work in with as well.
Regards
Andrew Orr
-No Stone Left Unturned
-Master of Women’s Health Medicine
-Master of Reproductive Medicine
-The Women’s Health Experts
Sex Around The Time of Embryo Transfer Increases The Likelihood of Successful Early Embryo Implantation and Development.
Research has now shown that sex around the time of embryo transfer increases the likelihood of successful early embryo implantation and development.
Intercourse during an IVF cycle has the potential to improve pregnancy rates and there is adequate research to now back this up. We know that in animal studies, exposure to semen is reported to promote embryo development and implantation.
Intercourse may assist implantation
This is actually good news for humans as well as it shows that intercourse may act to assist implantation. Animal studies reveal that exposure to seminal plasma, the fluid component of the ejaculate, is particularly important for achieving normal embryo development and implantation. Animals that become pregnant through artificial insemination or embryo transfer without being exposed to seminal plasma have substantially lower rates of implantation than those exposed to seminal plasma (Pang et al., 1979; Queen et al., 1981; O et al., 1988; Flowers and Esbenshade, 1993), while rodents inseminated with spermatozoa prior to blastocyst transfer also have a higher rate of implantation compared with those not exposed to spermatozoa (Carp et al., 1984).
Intercourse may influence pregnancy success rates
A multicentre prospective randomised controlled trial was conducted through IVF centred around the world, including Australia. The study was conducted to determine if intercourse around the time of embryo transfer, or just before and embryo transfer in an IVF cycle, actually has the potential to have any influence on pregnancy success rates.
Participants in Australian IVF clinics underwent frozen embryo transfer (FET) and participants in Spain IVF clinics did fresh embryo transfer. Participants were randomised to either have intercourse, or to abstain from intercourse around the time of embryo transfer.
The study showed that there was no significant difference in the pregnancy rates between those couples that abstained and those that had intercourse. However, the portion of transferred embryos that made it to 6-8 weeks gestation was significantly higher in the women exposed to semen compared to those who abstained.
This landmark multi-centre international study showed that women who had sex around the time of embryo transfer, and who were exposed to semen around the time of embryo transfer, had increased likelihood of successful early embryo implantation and development.
Couples need to be having more sex during IVF cycles
One of the things that I always promote as part of my fertility program, is that regular sex is so important for our fertility patients, on many levels. Sometimes the obvious eludes some people though.
One of the things we see quite regularly is that couples doing Assisted Reproduction (ART) are abstaining from sex fearing it will affect their chances of conceiving. Actually the opposite is true. By not having sex during ART cycles (IUI, IVF etc) you are affecting your chances of conception.
I have spoken about the importance of sex and orgasm assisting implantation in other posts and there is so much medical research to back this up. This is seen in the research I have talked about above.
Let’s be real and look at the facts
Let ask the question “If you were trying naturally, would you stop having sex for fear that conception has taken place?”
Then why would you stop having sex around an ART cycle?
Let’s face the facts, implantation takes place in the uterus, and not the vagina, and no man is that well endowed to even penetrate the cervix, so…. Let’s get a grip here
The question to ask is “What does an embryo feed off and need to successfully implant?”
The answer is blood!
Think of a tick borrowing into skin to feed off its host.
How do you get blood flow into the uterine lining?
The answer is that sex and climax stimulate blood flow to the lining to assist implantation and also prepare the lining for implantation. Nature has given us all the tools for healthy conception to take place, and yet many of us just aren’t using them.
Sex is more than just and egg and a sperm
Don’t forget that regular sex during this time not only helps assist implantation, but it also helps with the bonding process and physical connection process during this stressful time. Many couples split up because of losing this connection during the ART process and sex is a way of keeping that physical and emotional connection. Sex also tells your body you are also preparing to conceive on another level too.
For those doing IVF etc, next time you are doing an ART cycle maybe it is time to start doing things the way nature intended to give you that boost you so desperately are needing. Go get busy people
Final Word
If you are struggling to fall pregnant, or need advice with preconception care, please give my friendly staff a call and find out how my fertility program, which has helped over 12,500 babies into the world, may be able to assist you too.
Regards
Andrew Orr
– No Stone Left Unturned
-Master of Reproductive Medicine
-Master of Women’s Health Medicine
-The International Fertility Experts
References:
- http://humre.oxfordjournals.org/content/15/12/2653.short…
- Bellinge, B.S., Copeland, C.M., Thomas, T.D. et al. (1986) The influence of patient insemination on the implantation rate in an in vitro fertilization and embryo transfer program. Fertil. Steril. , 46, 252–256.
- Carp, H.J.A., Serr, D.M., Mashiach, S. et al. (1984) Influence of insemination on the implantation of transfered rat blastocysts. Gynecol. Obstet. Invest. , 18, 194–198.
- Coulam, C.B. and Stern, J.J. (1995) Effect of seminal plasma on implantation rates. Early Pregnancy , 1, 33–36.
- Fishel, S., Webster, J., Jackson, P. and Faratian, B. (1989) Evaluation of high vaginal insemination at oocyte recovery in patients undergoing in vitro fertilization. Fertil. Steril. , 51, 135–138.
- Franchin, R., Harmas, A., Benaoudia, F. et al. (1998a) Microbial flora of the cervix assessed at the time of embryo transfer adversely affects in vitro fertilization outcome. Fertil. Steril. , 70, 866–870.
- Franchin, R., Righini, C., Olivennes, F. et al. (1998b) Uterine contractions at the time of embryo transfer alter pregnancy rates after in-vitro fertilization. Hum. Reprod. , 13, 1968–1974.
- Marconi, G., Auge, L., Oses, R. et al. (1989) Does sexual intercourse improve pregnancy rates in gamete intrafallopian transfer? Fertil. Steril. , 51, 357–359.
- Pang, S.F., Chow, P.H. and Wong, T.M. (1979) The role of the seminal vesicles, coagulating glands and prostate glands on the fertility and fecundity of mice. J. Reprod. Fertil. , 56, 129–132.
- Qasim, S.M., Trias, A., Karacan, M. et al. (1996) Does the absence or presence of seminal fluid matter in patients undergoing ovulation induction with intrauterine insemination? Hum. Reprod. , 11, 1008–1010.
Regular sex found to trigger ovulation in females & make them more fertile.
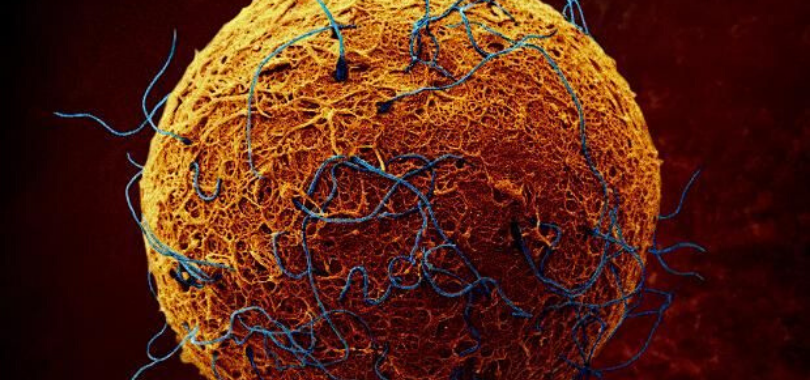
Regular sex isn’t just beneficial for ones health, physical and mental well being and happiness. Researchers have now found that regular sex and a protein in seminal fluid actually helps to trigger ovulation in females and make them more fertile to sustain a pregnancy.
Semen isn’t just a vehicle for carrying sperm
Semen isn’t just a vehicle for carrying sperm and studies actual now show that it also plays a crucial role in triggering ovulation. Researchers have discovered the protein in the seminal fluid acts as a hormonal signal on the female brain. This triggers the release of other hormones that signal the ovaries to release an egg.
The international team of researchers at the University of Saskatchewan, found this protein in a variety of mammals and say it plays an important role in reproduction in all mammals.
Male mammals have accessory sex glands that contribute seminal fluid to semen, but the role of this fluid and the glands that produce it are not well understood. From the results of the research, it is now understood that these glands produce large amounts of a protein that has a direct effect on the female brain and reproductive organs.
Ovulation Inducing Factor (OIF)
The protein, which was dubbed the ‘ovulation-inducing factor’ (OIF), works through the hypothalamus of the female brain. This part of the brain links the nervous system to the endocrine system (a system of glands that secrete hormones into the blood stream) via the pituitary gland.
The idea that a substance in mammalian semen has a direct effect on the female brain is not a new one, but now there is research to back these theories up. The scientists also discovered it is the same molecule that regulates the growth, maintenance, and survival of nerve cells.
OIF affects ovulation and fertility
In this study, they also looked at how OIF not only affected ovulation in females, but how it also affected their fertility and chances of a pregnancy.
For the purposes of the study, the research team looked at two species of mammals, that being llamas and cattle. They did this because Llamas are ‘induced ovulators, meaning that they ovulate only when they have been inseminated. Cows and humans on the other hand are ‘spontaneous ovulators,’ meaning that a regular build up of hormones stimulates the release of an egg.
Using a variety of techniques, the researchers found OIF present in semen samples taken from both animals. However, when they injected the llamas with this protein it caused them to ovulate. The same effect wasn’t seen in cattle.
While OIF didn’t appear to induce ovulation in spontaneous ovulators, such as cows and human, it did affect fertility in different ways. The protein was found to effect the timing of when cattle developed follicles (fluid-filled sacs in the ovary which carry the eggs). The researcher also found that OIF promoted the development of a temporary endocrine structure needed to sustain pregnancy.
Research has broaden our understanding of ovulation and fertility
This research definitely helps to broaden our understanding of the mechanisms that regulate ovulation and also helps to raises some interesting insights into fertility. More research is needed to see what role OIF plays in human fertility, as the researchers suspect it will be exactly the same. The study appeared in the Proceedings of the National Academy of Sciences.
It is great to see this research getting out there and this is something that I have promoted and taught for ages. It is great to see actual research to back up what I have teaching for years. Let’s face it, many of our advancements in fertility have actually come from veterinary science through use of IVF in cattle.
Couples undergoing IVF need to be having more sex
This is also great research that showed why couples trying to have a baby, or undergoing fertility treatments (IVF etc) need to still be having sex. It isn’t rocket science, yet so many people forget basic biology and that we are actually still an animal.
The problem is that so many couples actually stop having sex when doing assisted reproduction such as IVF. While I can totally understand the whole emotional aspect of why, it is still hindering their chances of conception and having a successful pregnancy. It is a truth that must be talked about and also get couples to understand.
Regular sex also helps with connection for the couple
I am always telling them how important it is to still have an active sex life, for the benefit of a happy, healthy relationship. It is also about the connection and not just about having sex. We do see so many couples split up while undergoing IVF and assisted reproduction, and some of this is purely due to lack of bonding and connection with their partner.
But even so, regular sex and intercourse also gives the chance of a natural pregnancy too, no matter how slim the chance for some couples. We still see couples that have done multiple cycles of IVF still conceiving naturally, but you actually have to have sex for this to happen.
Now we have research, which shows that a protein in seminal fluid actually acts as a hormonal signal that actually triggers ovulation, improves egg quality and may in fact make a woman more fertile for a pregnancy to take place. Again, when you look at this logically, it really is not rocket science and really is easy to understand.
Regular sex while doing IVF improves pregnancy rates.
This is why it is so important for all our couples using ART (Assisted Reproduction Therapy) and IVF to still keep having sex. Regular sex and more importantly regular climax, increases your sex hormones, helps regulate hormones, increases blood flow to the uterine lining, helps with libido, helps with egg quality, helps for better ovulation and most of all improves your fertility and the chance of sustaining a pregnancy. There is also research to show that regular sex before and after IVF transfer, improves pregnancy rates and I will talk about this research in another article on it’s own.
Final Word
If you are struggling to have a baby, and need help with fertility issues, then talk to my friendly staff about how our fertility program might be able to assist you. It has helped over 12,500 babies into the world… and counting.
Regards
Andrew Orr
-No Stone Left Unturned
-Master of Reproductive Medicine
-Master of Women’s Health Medicine
-The International Fertility Experts
Frequently asked questions about screening for ovarian cancer
I have recently put up a post about ovarian cancer and as usual lots of people had question about the symptoms and also about proper screening. Just like many other serious health issues, there are lots of myths out there and why it is important to talk about the facts only.
Before I go into the frequently asked questions about screening for ovarian cancer, I do need to say this. If you do have bloating, or some of the other common symptoms of ovarian cancer, please don’t get all anxious and run off thinking you have ovarian cancer.
Many of these symptoms can be indicative of endometriosis and adenomyosis too. This is why it is important to talk to your healthcare practitioner, or specialist about any concerns you have around any of the symptoms you may be getting. Early intervention and detection is the key to any disease, and ovarian cancer is exactly the same. Either way it is worth seeing someone a specialist in this field.
If you do have any of the symptoms from my post on ovarian cancer, please talk to your healthcare practitioner about a referral to an expert, or specialist in this field and get assessed properly.
Frequently asked questions about ovarian cancer screening
This information covers screening for ovarian cancer i.e. the testing of women at population risk who have no symptoms that might be ovarian cancer. This information has been developed to support discussion with a woman about screening for ovarian cancer. Most of this can be found at the Australian Cancer Council (www.cancer.org.au)and the National Breast and Ovarian Cancer Centre (www.nbocc.org.au)
Is there a screening test for ovarian cancer?
No. There is currently no evidence to support the use of any test, including pelvic examination, CA125 or other biomarkers, ultrasound (including transvaginal ultrasound), or a combination of tests, to screen for ovarian cancer.
A Pap test does not detect ovarian cancer; it is only used to screen for cervical cancer.
What about the CA125 blood test?
CA125 is a protein found in the blood. It is known as a tumour or cancer marker. Increased levels of CA125 may indicate ovarian cancer. However, there are many other conditions that can affect CA125 levels such as ovulation, menstruation, endometriosis, benign ovarian cysts, liver or kidney disease, and other cancers such as breast or lung cancer.
If CA125 levels are not raised, this does not completely rule out ovarian cancer, as about 50% of women with early-stage ovarian cancer have normal CA125 levels.
For these reasons, the CA125 test alone should not be used as a screening test for ovarian cancer. It can be used in the assessment of symptoms that may be ovarian cancer.
Can an ultrasound be used as a screening test?
A transvaginal ultrasound (TVUS) gives the best picture of the ovaries but while able to detect the presence of ovarian disease, a TVUS cannot distinguish between benign and malignant disease.
For this reason, transvaginal ultrasound should not be used as a screening test for ovarian cancer.
What if a woman decides she still wishes to have a CA125 blood test or ultrasound?
She should be informed that if either a CA125 or an ultrasound test is abnormal, it may be necessary to repeat the test, or to undertake further tests, which may include surgery to investigate the abnormal result.
The discovery and investigation of abnormal findings can result in unnecessary anxiety and the investigations can carry significant risks.
Final word
I hope this explains a few of the fact around screening for ovarian cancer and helps people understand why some perceived screening methods are not reliable. For more information, you should always talk to your healthcare practitioner, or specialist, and never ever diagnose yourself based on some stupid google search. Always see a qualified healthcare professional for all your healthcare advice. Your life could depend on it.
Regards
Andrew Orr
-No Stone Left Unturned
-Master of Women’s Health Medicine
-Master of Reproductive Medicine
-The Women’s Health Experts
The Link Between Endometriosis & Cancer
One of the most common questions that I get asked from women with endometriosis is “Is there a link between endometriosis and cancer?”
There has been many research papers on this and there is some evidence to suggest that women with endometriosis may have a higher risk of certain cancers such as endometrial cancer and also ovarian cancer.
We all know that Endometriosis is a debilitating disease, but many people don’t realise the possible future implications of this disease, mixed with our highly inflammatory diets and lifestyle. Unfortunately it is a recipe for any inflammatory disease, and for expression of cancer cells.
There have been many reputable studies to date showing the link between inflammation and cancer and endometriosis is definitely an inflammatory disease that needs proper management otherwise some studies are now suggesting it could be a precursor to certain cancers.
This isn’t meant to scare anyone either. It is just to help people realise the possible implications of this disease and to be more proactive around getting yourself and your body healthier and also being properly managed by a qualified health professional. When it come to cancerous states, prevention is key and early intervention is also.
Better education is needed
Given that, we need to really take this disease more seriously than many people with the disease and many in the medical community probably realise. Prevention is always the key to any disease and even though endometriosis cannot be prevented, early intervention and ongoing management of the disease is crucial. This is why I think all young girls should be educated about what a proper menstrual cycle should be like and that period pain is not normal. There also needs to be proper education about diet and lifestyle interventions with inflammatory diseases, such as endometriosis, and how it also needs a multimodality approach to be managed properly.
Endometriosis is like cancer in many ways
Endometriosis, like cancer, is characterised by cell invasion and unrestrained growth. Furthermore, endometriosis and cancer are similar in other aspects, such as the development of new blood vessels and a decrease in the number of cells undergoing apoptosis. In spite of these similarities, endometriosis is not considered a malignant disorder.
The possibility that endometriosis could, however, transform and become cancer has been debated in the literature since 1925. Mutations in the certain genes have been implicated in the cause of endometriosis and in the progression to cancer of the ovary (Swiersz 2006). There is also data to support that ovarian endometriosis could have the potential for malignant transformation. Epidemiologic and genetic studies support this notion. It seems that endometriosis is associated with specific types of ovarian cancer (endometrioid and clear cell) (Vlahos et al, 2010). The relationship between endometriosis and ovarian cancer is an intriguing and still poorly investigated issue. Specifically, histological findings indicate a definitive association between endometriosis and endometrioid/clear cell carcinoma of the ovary (Parihar & Mirge 2009).
Women with endometriosis may be more prone to certain cancers
There are recent studies which have shown that mutations in the certain genes found were identified in 20% of endometrial carcinomas and 20.6% of solitary endometrial cysts, played a part in the development of ovarian cancers. In addition to cancerous transformation at the site of endometriosis, there is recent evidence to indicate that having endometriosis itself may increase a woman’s risk of developing non-Hodgkin’s lymphoma, malignant melanoma, and breast cancer (Swiersz 2014).
Women with endometriosis appear to be more likely to develop certain types of cancer. Brinton, PhD, Chief of the Hormonal and Reproductive Epidemiology branch at the National Cancer Institute has studied the long-term effects of endometriosis, which led her to Sweden about 20 years ago. Using the country’s national inpatient register, she identified more than 20,000 women who had been hospitalised for endometriosis.
After an average follow-up of more than 11 years, the risk for cancer among these women was elevated by 90% for ovarian cancer, 40% for hematopoietic cancer (primarily non-Hodgkin’s lymphoma), and 30% for breast cancer. Having a longer history of endometriosis and being diagnosed at a young age were both associated with increased ovarian cancer risk (Brinton et al, 1997).
Farr Nezhat, MD, Chief of Gynecologic Minimally Invasive Surgery and Robotics at St. Luke’s and Roosevelt Hospitals in New York City and Professor of Obstetrics and Gynecology at Columbia University, spoke on the pathogenesis of endometriosis and ovarian cancer. According to a 2000 study of women with ovarian cancer by Hiroyuki Yoshikawa and colleagues, endometriosis was present in 39% of the women with clear cell tumours and 21% of those with endometrial tumours. The studies clearly suggest that Endometriosis may be the precursor of clear cell, or endometrial ovarian cancer (Yoshikawa et al, 2000).
Inflammation and Estrogens are a big factor in many cancers
If you combine inflammation with oestrogen as with both endometriosis and ovarian or uterine cancers, it’s going to be a vicious circle, as the 2 diseases share numerous other characteristics. For example, both are related to early menstrual cycles and late menopause, infertility, and inability to fall pregnant. Any factors that relieve or offer protection against both conditions need to be explored, including dietary and lifestyle changes etc.
Some authors also suggest that there is an also increased risks of colon cancer, ovarian cancer, thyroid cancer non-Hodgkin’s lymphoma and malignant melanoma in women with endometriosis when compared with the general population (Brinton et al, 2005).
Proper management and early intervention is crucial
If you do have patients with endometriosis you do need to take into consideration the future implications of this disease, not only the pain and turmoil it causes on the way, but also the future possibility that endometriosis could also lead to cervical cancer, ovarian cancer, or many of the other cancers that can be found in the body.
There are certain medications, both natural based and medical that can great assist in the treatments and management of endometriosis and microscopic endometriosis implants. These do need to be explored and we now have the Royal College of Obstetricians and Gynaecologists recommending diet and lifestyle changes and to use complementary medicine such and Chinese Herbal Medicine and Acupuncture for the the management and treatment of endometriosis. This is recommended alongside medical interventions and it does get back to a multimodality approach is the key factor in proper management of this disease.
Diet and lifestyle changes are crucial in cancer prevention
There have been numerous studies showing the benefits of a low inflammatory based diet and reduction in lifestyle factors such as stress. These things are also crucial in any inflammatory disease and certainly in cancer prevention.
Anyone with endometriosis does need to be following anti-inflammatory diet, with reduced refined foods and increased whole foods. This is something I promote whole-heartedly and see great results with on a daily basis. It is also part of my PACE- Diet and Lifestyle program. PACE meaning (Paleo/Primal Ancestral Clean Eating) .
This style of diet is very much like the mediterranean diet which is now shown to be one of the best diets in the world to help with cancer prevention and reduction of cardiovascular disease. It is something that has been shown to assist with inflammatory diseases such as endometriosis. This can be done alongside supplements such as omega 3 oils and antioxidants that also offer protection and prevention against inflammatory diseases too. You should also talk to a qualified healthcare professional about diet and lifestyle interventions and supplementation.
See an Endometriosis Expert
Hope that helps everyone to understand why it is so important to really make some proactive changes if you do have endometriosis. You really need to explore as many options as you can when trying to manage this disease and halt its progression. It is also important to see an endometriosis expert and not try and manage this disease yourself. You just should not be doing this and it is not effective management. Always see an appropriately trained healthcare professional who is trained in endometriosis and other disease states in women. We don’t want to see it end up as cancer later on and this is why it is so important to make sure you are being appropriately managed now.
Final Word
If you do need help with endometriosis, and the associated symptoms of endometriosis, give my friendly staff a call and find out how I can help you. Always remember that early intervention is the key and being managed properly is also crucial.
Take care
Regards
Andrew Orr
-No Stone Left Unturned
-Master of Reproductive Medicine
-Master of Women’s Health Medicine
-The Endometriosis Experts
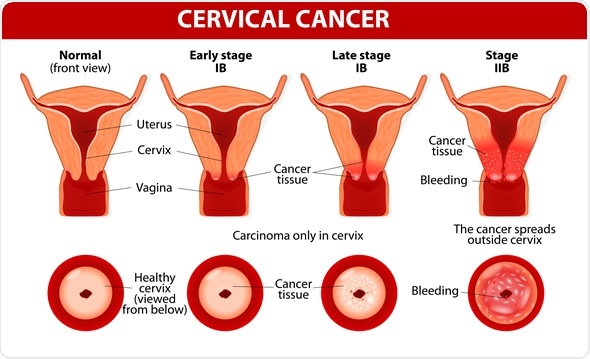
Cervical Cancer Awareness
Cervical cancer awareness is something all women need to know about and why proper screening for women is so important. It is so important that we bring awareness to cervical cancer, just as we do to many other cancers such as breast cancer and ovarian cancer.
Cervical cancer remains a significant cause of death, from cancer in women worldwide. In clinic I see so many women with the early, intermediate and sometimes advanced stages of cervical cancer. It isn’t good and many women with early detection on cancer cells aren’t being proactive in follow up consults, or have little idea just how significant these results are to their future health and possible length of their life.
Our increasing understanding of the relationship between HPV infection, pre-invasive and invasive disease of the cervix, the introduction of population screening programs using Pap smear testing, the availability of HPV vaccines, and the introduction of testing for high-risk HPV DNA types have changed the burden of disease in developed countries but even so, cervical cancer remains a significant problem in developing countries.
The Statistics of Cervical Cancer
World wide, cervical cancer is the fourth most common cancer in women, and the 7th most common overall.
In 2012, there were approximately 528 000 new cases of cervical cancer, and there were 266 000 deaths as a result of cervical cancer. In 2015, there were 857 new cases of cervical cancer diagnosed in Australia. In 2019, it is estimated that 951 new cases of cervical cancer will be diagnosed in Australia. In 2019, it is estimated that the risk of a female being diagnosed with cervical cancer by her 85th birthday will be 1 in 494.
The majority of cases (approximately 85%) and deaths (87%) occur in less developed regions.
In Australia a report by the AIHW “Gynecological Cancers in Australia: an overview” showed the following statistics regarding cervical cancer.
-there were 951 cases of cervical cancer, accounting for 1.4% of all gynaecological cancers
– cervical cancer was the 14th most commonly diagnosed cancer in females
– the estimated number of deaths from cervical cancer was 256
– approximately 70% of cervical cancers were diagnosed in women under the age of 60 years
– the risk of being diagnosed with cervical cancer by the age of 85 years was 1 in 494.
HPV and cervical cancer
HPV (Human Papilloma Virus) is a major cause of cervical cancer and why we need to get the safe sex message out there. In a study of almost of 1000 cases of cervical cancer worldwide, the prevalence of HPV infection was 99.7%.
Screening and regular checkup are also needed in the overall prevention and early intervention of this disease. Large population based studies have shown that screening via gynaecological examinations and Cytologic (Pap smear),may decrease cancer incidence and mortality by more than 80%.
The current screening recommendations are:
Routine screening with Pap smears use to be carried out every two years for women who have no symptoms or history suggestive of cervical pathology. Since 2017, the pap test has been done away with and that has now changed to the new cervical screening test.
All women who have ever been sexually active should start having Pap smears between the ages of 18 and 20 years, or one or two years after first having sexual intercourse, whichever is later. In some cases, it may be appropriate to start screening before 18 years of age.
Pap smears may cease at the age of 70 years for women who have had two normal Pap smears within the last five years. Women over 70 years who have never had a Pap smear, or who request a Pap smear, should be screened.
This policy applies to women with no symptoms and normal Pap smear results who should be screened. To find out more about the cervical screening test, you should talk you your healthcare practitioner, or specialist. You can also find out more information about cervical cancer screening at Cancer Australia
National screening and education about regular screening, has had a significant impact on the reduction of cervical cancer and deaths caused by this disease
HPV Vaccination
Please note that HPV vaccinated women would still require cervical screening as the HPV vaccine does not protect against all the types of HPV that cause cervical cancer. Until any changes are implemented women should continue to have two yearly Pap tests.
Symptoms of Cervical Cancer
Abnormal vaginal bleeding is the most common symptom of invasive cancer of the cervix. This may include bleeding after sex, bleeding in-between periods, or post-menopausal bleeding.
Cervical cancer is often asymptomatic until quite advanced in women who are not sexually active.
Other symptoms may include:
- Pelvic pain
- Bowel or bladder symptoms due to pelvic pressure
- Symptoms from a fistula (leaking urine or faeces vaginally)
Cervical cancer is preventable
Cervical cancer remains an important preventable cause of cancer in women both in Australia and worldwide. Even with the advent of vaccines, it is very important to remember that participation in regular screening is still necessary and a key part of reducing the incidence and deaths from cervical cancer.
Avoiding risk factors and increasing protective factors will help prevent many forms of cancer
The following risk factors increase the risk of cervical cancer:
1. HPV infection
2. Smoking (even social smoking, or 1-2 per day)
3. DES (diethylstilbestrol) Exposure – A man made estrogen
4. Poor diet
5. Being Overweight
6. Lack of exercise
7. High number of full-term pregnancies
8. Long term use of oral contraceptives
The following protective factors decrease the risk of cervical cancer:
1. Preventing HPV infection
2. Cervical Cancer Screening (pap smears & new HPV screen)
3. Diet (decreasing highly refined foods)
4. Exercise
5. Weight Loss
6. Quitting smoking
Avoiding risk factors and increasing protective factors does help prevent cancers and we all need to look at avoiding the risk factors and increasing more of the protective factors. If you are worried about your risks, you should talk to your healthcare professional about how you might lower your risk of cervical cancer.
Final Word
In practice I see so many women presenting with various stages of this disease and end up not being pro-active around the treatment of the disease. So many take this disease and precancerous cells too lightly. It can kill if not treated properly and therefore it is important to follow up with proper screening, treatments and interventions of cervical cancer.
Let’s bring more awareness to cervical cancer and let’s bring more awareness to prevention and hopefully a cure.
Regards
Andrew Orr
-No Stone Left Unturned
-Master of Women’s Health Medicine
-The Women’s Health Experts
Breast Cancer Awareness
Breast cancer awareness is something that everyone should know about. Mankind has known breast cancer since ancient times. In 460 B.C. Hippocrates explained breast cancer as a disease caused by an excess of black bile, or “Melancholia”. He named the condition ‘Karkinos’- (Cancer)- the Greek word for crab and the astrological constellation. This was because the tumor seemed to have tentacles which reached out into the surrounding breast tissue, resembling the legs of a crab.
The history of Breast Cancer
This theory of Hippocrates held for many centuries until 1680, when the French physician Francois de la Boe Sylvius suggested that Breast Cancer developed from an increase in the disruptions of the acidity of local lymphatic fluids.
There were many theories that followed including celibacy causing breast cancer, too much rigorous sex causing disruption to the local lymph drainage and thus causing breast cancer and others linking breast cancer to mental disorder-the melancholia references again.
In 1757 Dr Henri Le Dran was the first person to suggest that the surgical removal of the tumor was the most effective treatment, provided all the lymph nodes in the armpits were removed. This must have been a horrific prospect prior to anaesthetic and proper sterilised surgical procedures. The survival rates were appalling, due to immediate death post surgery from the high infection rates. It wasn’t until 1976 that advancement in radiation and chemotherapy actually took place. This really isn’t that long ago and the first mammogram trails showing reduction of breast cancer due to early screening, where only initiated in 1989. To think that in such a short spam of time, we now have this as a routine screening tool that can save lives.
It wasn’t until 1994 that scientist have isolated the first of the genetic mutations associated with breast cancer and these genetic screening for the gene mutations and being predisposed to breast cancer. This screen has led to Angelina Jolie having a double mastectomy when testing revealed she had the BRCA1 gene mutation which predisposed her to both ovarian and breast cancer. It was estimated that Jolie had an 87% risk of breast cancer and a 50% risk of ovarian cancer. Jolie’s mother died at 59 from the disease in 2007.
Since Angelina Jolies decision, there was a surge in enquiries around genetic testing and medical evaluation as to breast cancer risks across all parts of the world.
Breast cancer remains the most common malignancy in women, comprising 18% of all female cancers and there is 1 million cases of breast cancer diagnosed worldwide. Most women will know someone who has had the diagnosis, based on these figures.
Despite all the testing and screening it is estimated that about 40% of women have never discussed their risk factors with there doctor, or health care practitioner.
So what can you do to reduce your risks?
The first thing anyone can do is check yourself for any noticeable signs of changes to the breast. You can also have a routine breast examination at your doctor.
Next is regular mammogram, or ultrasound screening, followed by biopsy if anything suspicious is found. Screening for genetic predisposition is another tool that should be used by all women too. About 10% of breast cancer in developed countries is due to genetic predisposition. Certain populations of people have higher genetic risk factors with the Ashkenazi Jewish population having the highest risk factors and well as risk factors for some rare genetic diseases.
The good thing with early screening and detection is that we have now seen in increase in survival rates with the increase between 72-89%.
There are also other risk factors that people need to take into consideration. Women who have their menstrual cycle too early and those who go into menopause later in life are at increase risk of developing breast cancer. Having a baby later in life also increases the risk factor for cancer. Having a baby after 35 years old doubles the risk, while having children earlier reduces the risk. Breast-feeding also reduced the risk of breast cancer too.
Obesity and lifestyle factors increasing breast cancer risks
Obesity and increased alcohol intake also increases a woman’s risk and doubles the chances of having breast cancer. Obesity doubles a woman’s risk factors in postmenopausal women and increased alcohol intake (3-6 standard drinks per day) also doubles the risk factors.
Women on the combined pill also have in increased risk of breast cancer, while progesterone only options do not increase the risk.
Lifestyle modifications
Since there is compelling evidence alcohol and obesity increase the risk of breast cancer, women do need to reduce their alcohol intake and also aim to keep their weight within a healthy range.
This is why we all need to be looking at anti-inflammatory based diets, free from inflammatory wheat grains, excess refined soy products, alcohol, refined foods and refined sugars. These highly inflammatory based foods all lead to excess blood sugars, which in turn spike insulin product. This then causes interference to hormone metabolism (namely estrogens) and also causes the body to store fats and stops the burning of fats, again interfering with estrogen metabolism. This is turns causes inflammation, which is he cause of many of our disease states and leading causes of death.
This is why I always promote a Primal based, low inflammatory, clean eating diet. This is the basis for my PACE-Diet and Lifestyle program (Paleo/Primal Ancestral Clean Eating) that I promote to my patients. This style of diet promotes leans meats, fresh fruits, nuts, seeds, good fats, fresh vegetables and salads, clean water etc. This is very similar to the famous Mediterranean diet, which has to date never been scrutinized and has lot of research behind it. Eating this way will not only make you healthier for it, but will be reducing your risk factors around any inflammatory disease state. Just remember that 90% of breast cancers come from non-hereditary factors related to lifestyle and the way we eat in the modern world.
Early detection and awareness is vital
It is well known that early detection and treatment is vital to survival rates in women with breast cancer. It is so important to regularly check for lumps and bumps and talk to your doctor about regular screening. If you have hereditary risks then talk to your healthcare provider, or specialist about genetic screening for breast cancer.
Let’s all raise awareness for breast cancer and support more research into finding a cure for this disease that affects millions of women world wide each year.
Regards
Andrew Orr
-No Stone Left Unturned
-Master of Women’s Health Medicine
-The Women’s Health Experts
Bringing Awareness To Cancers In Women
Over the next week I am going to focus on a very serious subject – Cancers in women.
Having recently focusses on the awareness of endometriosis and adenemyosis, I thought I should bring some awareness to the topic of cancers in women as a whole. This isn’t to scare people either. It is to bring awareness to a very serious topic and to help people understand the importance of early intervention and changes to diet and lifestyle can greatly reduce the risks of this horrible disease.
With cancer rates increasing I am going to focus on the cancers that affect the female reproductive system and impact of reproductive health. This will also include those cancers that increase after menopause too. Whenever I talk about fertility and reproduction, it is referring to the stage in life when women are fertile and are of reproductive age. Menopause is also including because that still comes under the reproductive system.
Cancer has been around a long time
Humankind has been dealing with the impact of cancer and malignancy for its entire history and the first clear description of any cancer is found in the Ebers Papyrus, dating from nearly 3500 years ago. The cancer was very accurate described by the Egyptian writer and what was described was in fact breast cancer. Chinese Medicine has texts dating back for further than that, describing the different forms of cancers and their treatments. Modern medicine does tend to only reference Greek, Egyptian and Roman text.
When these Greek physicians first cut the surface of a breast cancer, it did in fact resemble a crab, because of it solid central body, with extensions into the surrounding tissue resembling legs.
The ancient Greek word for crab is “Karkinos” which in Latin is translated into ‘cancer’- as in the astrological sign. This term was then extended into all cancers and malignancies, not just breast cancer.
Genetic, hereditary and hormonal links to cancer
It is believed that cancer is predominantly caused by a failure in the regulation of genes which govern cell growth and differentiation. Malignant change is most typically the result of a cascade of changes in a number of genes.
These changes in genes can be bought on by hereditary genetic genetic changes, while others may be the incorporation of foreign viral DNA, or a compound that may act as the primary trigger for malignant change. Some cancers and malignancies are also caused by hormonal stimulation both internally and by injection, or ingestion of hormones from an outside source (Drugs, Hormone Replacement etc).
Diet and lifestyle links to cancer
Other cancers are plain and simply caused by the highly inflammatory foods we eat and the lifestyle we live. Obesity and being overweight increases our cancer risks and there are no many studies proving these links. Having excess fat stores, eating highly processed foods, high GI foods and over 3-4 glasses of alcohol per week can increase your cancer risks exponentially. This why we all need to adopt a clean eating approach to foods and look at eating less refined foods and more whole foods.
The incidence of cancers in women is highest in developing western countries and lowest in countries such as Africa and Asia. The difference has more to do with diet than it does genetics. Since there is compelling evidence that alcohol, highly refined foods and obesity increase the risk of cancers in women (and men) I will be focusing greatly on the need for us all to look at changing our diets to not only help in the prevention of certain cancers, but to also help prevention of other disease states that are leading causes of our lives being cut short.
The most common cancer in women
Since breast cancer remains the most common malignancy in women, comprising of 18% of all female cancers, most women will know someone who has had this diagnosis.
I’ll focus on breast cancer firstly and then go into the other cancers so that we can all be educated about how we can prevent these disease states from increasing. If you have any questions, or topics you want discussed around this topic, please let me know
Take care and remember prevention is better than cure. Always talk to your doctor, or healthcare practitioner about cancer risks and always seek early intervention if you find any lumps and bumps that were not there before.
Hope you the topics help you all. If I can save just one person with this information, then I am happy. Lets try and save more than one, so please like and share to spread the word.
Regards
Andrew Orr
-No Stone Left Unturned
-Master of Women’s Health Medicine
-The Women’s Health Experts