Explaining endometriosis to people is not always easy and sometimes you have to use analogies that seem strange at first, but once you get the gist of where I am going with it, it will all make sense. But before I start, I always like to say that please take the personal out of things and just know that what ever analogy I use, it is with good intention and always about helping others.
I just know that when I used the “Endo is like Rust” analogy, which is what it is like, a few people took it to heart as though they had a rusty uterus and this is not what I was saying. Not at all.
Please know that I have loved ones with this horrible disease, so I am here to help, and my main aim now is to help as many people as possible with what I know, and how to treat people properly. I am also about getting the message out there so that women to not have to remain silent about this disease any longer. My motto is, and always will be, “Period Pain is Not Normal”
So, sit back, take out the personal and know that I am writing from a place of caring and sharing and a place of getting the message out there to help you all. Sometimes you just have to tell it how it is, in order for people to sit up and listen, so here we go J
Many of you have read my article of “Rust Never Sleeps and Neither Does Endometriosis” and the reason I wrote this is because endometriosis and how it attacks the body, is very much like how rust attacks metal. If you haven’t read the article, please do so that you can see what I am trying to convey.
I am always doing lots of speaking events and seminars on Women’s Health and also presenting for workshops on Endometriosis. It is so great to get the message out to the world, so that both the public and healthcare professionals can be educated on this subject better.
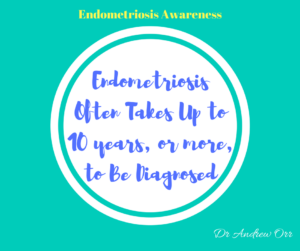
We need to stop having this disease “Missed” and women being “Dismissed” as I am always saying now. This disease should not be taking 8 years from onset to definitive diagnosis. It used to be 12 years. This is disgusting, to say the least, and there is no excuse for this to be happening, except poor education, sloppy diagnosis, lack of training, negligence and dismissive egos that need an attitude adjustment.
But, in saying that, we also need to teach women to be empowered and not just put up with being told “This is normal”, or “Just go on the pill and it will fix it”. That is bullshit (sorry). But it is true. There needs to be a better way and we need to stand up and say “Enough”. But we also need to not let the disease define you and get caught up in the blame game either.
We also need to get people to stop “Dr Googling” too, as this is also spreading the misinformation. It is great to be educated, but good old “Dr Google” is full of false information and research shows that up to 75% of the health information that the public can access on google, is either wrong, or only partially true.
Now that I have had my little rant about the injustices of many, I would like to share what I have been sharing to others about what endometriosis is really like and how hopefully we can prevent it from returning, hopefully for good.
I do know this is possible with the right care, right follow up treatments and right team of people helping. I see it daily and know what I share to be true. But, again it requires the person to follow the advice given and then to get the information out there. It also requires people to not be defined by their disease and break free from these chains to open their minds to the possibilities of new thought, new treatments and new ways of doing things. We need to not be caught up in what may cause the disease, but what we can do to help those with it now.
Of course prevention is crucial and so important, but once the disease is expressed in the body, what caused it is irrelevant. We can argue about the hypothesis of what may be the initial causal factor until the end of time, but that isn’t helping those with the disease now. The most important factor is how we can help those with it live a normal life and hopefully one day in the future to be free of the disease completely. At least for now, we can look at hopefully giving people a better quality of life than the one they are living each day. From my experience, I do know that this is possible with the right team of people working the help the individual.
To be honest, the most likely cause of this disease is now known to be genetic links, or chromosomal, most likely through the parental mode of inheritance. Gene therapy is probably going to provide the biggest breakthrough in this disease in the years to come. But like any breakthrough, we just have to wait and see what happens there. You heard it here first. I do believe genetics does play a big part, but like any disease, it is not the only contributing factor.
But, all this aside, we need to focus on the here and now to help those who need help now. In order to make change, you need to make those changes required. If you change nothing, nothing will change. I also get how hard it is for those whom have suffered so long to pick themselves up, to make those changes. Believe me, as someone who has been through a major life threatening illness and pain and crawled their way back to good health and do what I do now, I get it. I’ve been to that point of wanting it all to just stop and I get what many women put up with on a daily basis. Pain is pain, no matter where it has stemmed from.
Getting back to the subject at hand, I have now been explaining that Endometriosis is like a weed. Why would I explain it like this?
Like a weed, endometriosis grows and spreads. You can physically remove the weed (surgically), but unless you control the regrowth, seeds have been dropped (endometriosis regrowth) and then the weeds pop up again and start to grow once more. Sound like endometriosis too you?
Like any weed, it needs certain things for its regrowth. We have just talked about the dropping of the seeds ( regrowth) but it needs a food and fuel source to make it grow (estrogens, insulin, inflammatory response from external factors, stress etc). Then once the seeds are fed, the regrowth continues and then the garden is infested with the weed plague once more. Then you need to try and physically removed the weeds again once more and so the cycle begins again. Are you seeing what I am getting at yet?
Just like these weeds, endometriosis is often removed and many people then either believe they are fixed, or they do not do anything post surgery to prevent that regrowth. Before they know it, they again have to go back for more surgery. Often when people do try to control the regrowth (Progestins, Mirena etc), they are only employing one method, for which is either not effective enough, or the weed (Endo) is now resistant too.
This is why we need to employ a multimodality approach post surgery to hopefully complete eradicate the weed regrowth and halt the life cycle of these seeds being spread and to start growing again, thus starting the horrible cycle all over again
Now that we can see how endometriosis is really like a weed that can spread throughout our garden, we need to look at what we can do to hopefully stop it coming back, or spreading into other parts of the body.
Like I said, treatment must be individualised, using a multimodality approach, taking the clinical problem in its entirety into account, including the impact of the disease and the effect of its treatment on quality of life. Pain symptoms may persist despite seemingly adequate medical and/or surgical treatment of the disease.
The real focus needs to be on prevention and treatment strategies post surgery. Even better still, lets prevent it before it starts
There is an ancient Chinese saying – “To try and treat a disease once it is fully expressed into the body is like trying to forge arms once a war has already started, or like trying to dig a well once you are already thirsty – Yellow Emperors Classics of Internal Medicine”
The same goes for endometriosis. Once the disease is there and expressed into the body, it is hard to treat, especially is known methods of treatment are failing and this individualised, multimodality approach is used.
A Multimodality Approach Should Include:
- Surgery
- Pain Management
- Hormone Therapy
- Counselling
- Lifestyle changes
- Exercise
- Pilates/Yoga
- Changes to Diet
- Traditional Chinese Medicine
- Acupuncture
- Holistic Medicine
- Anything people have tried and has worked for them
The Royal College of Obstetricians & Gynaecologist guidelines for the “Investigations and Management of Endometriosis” have the following quote:
“Many women with endometriosis report that nutritional and complementary therapies such as homeopathy, reflexology, traditional Chinese medicine or herbal treatments, do improve pain symptoms. They should not be ruled out if the woman feels they could be beneficial for her overall pain management and/or quality of life, or work in conjunction with more modern medical therapies.”
This is why it is vital to take careful note of the woman’s complaints and to give her time to express her concerns and anxieties, as with other chronic diseases, just as I do for all of my patients. Healthcare providers actually need to listen to the woman and her concerns. Women need to be listened to and be heard and be nurtured
It is also important to involve the woman in all decisions, to be flexible in diagnostic and therapeutic thinking, to maintain a good relationship with the woman and for healthcare providers to seek advice where appropriate from more experienced colleagues. This is something that I try to educate all my patients with and something I also try to educate healthcare providers with when I do my seminars and speaking events about Women’s Health issues and diseases like endometriosis.
But while there are thing that healthcare providers need to do, there also things you must do also. These include
- Reducing Stress
- Look at Emotions and How They Affect You
- Exercise
- Get “You Time”
- Eat more protein and less High GI Carbs
- Eat less process and package foods that we now call “Carbage”
- Loss some weight if you have excess fats (which spike estrogens)
- Gain some weight if you are underweight.
- Do Something You Love (At least once per week)
- Laugh Often (Even if some days you feel like crying)
- Spend Time With Friends and Loved Ones
- Make Love J ( Climax and Oxytocin are your friends)
- Do Not Let The Disease Define You
- Don’t Buy Into The Label
- You are more than this disease
- If something is helping, then continue with it, no matter what anyone tells you
- Just remember that “You” are uniquely “You”
Please remember these words :
- Do Not Let The Disease Define You
- Don’t Buy Into The Label
- You are more than this disease
- If something is helping, then continue with it, no matter what anyone tells you
- Don’t buy into everything you read on the internet, social media, or “Dr Google. To be honest, I ban “Dr Google” with my patient (haha)
- Make sure you have a good laugh each day, but remember it is also OK to have a good cry too
- It is OK to unplug every so often
- It is OK to take the “Superwoman” cape off every so often too.
- Remember “You” are uniquely “You”
This is why it is so important to not get caught up in what others have done, or tried and may not now be working for you either. We need to look at you as an individual and treat you as such. What works for one person, may not work for another. This is why an individualised multimodality approach is needed to help prevent and treat this horrible disease and we often need a team of people, on the same page, to help treat this properly.
Don’t forget to “Get A Second Opinion”, or a Third, or Fourth, or Tenth one if needed
In many other areas in life we will get multiple quotes, and opinions. Yet, when it comes to our health, we often only get one quote, or maybe two.
Just because someone has your history, or is nice to you, or maybe recommended by a friend etc, does not make them a good practitioner. It does not mean that you cannot get another opinion. If someone isn’t helping you, then you need to look at changing, no matter who they are, or how well they know your history.
Not every specialist you see is a good surgeon either, so please remember this. You need to have someone who specialises in endometriosis and who has done advanced surgical training, not just minimal training. There is good and bad in every profession and the medical profession is not exempt from this either.
The complementary medicine profession, or allied health care profession exempt from this either. Your health is important and so is the value of another opinion. Not every practitioner has all the answers. If someone isn’t helping you, then don’t be scared to change.
Lastly please remember to know that there is always help out there. I am always here to help people as well. I have a special interest in endometriosis and do a lot of education and research into this disease. I also have masters level post graduate training in this disease and other women’s health and reproductive conditions.
You can always come and see me in person, or make an initial online consult (zoom) for those who live at a distance. I have a great team of people I work with to give you the best help possible. I have a team of some of the best health care professionals and I make sure all of the team I work in with, are at the top of their game in their chosen profession.
Let me be the conductor of your health issues and help you get the treatment and advice you so desperately deserve. I am here to listen to you and hear you. I make sure you don’t have things “Missed” and aren’t “Dismissed “ and why my treatment motto is “Leaving No Stone Unturned”. I am out there as a voice for women and being a crusader for women’s health everywhere. I don’t mind stepping on a few toes, and ego’s to get you the best help possible J
Take care and remember that “Period Pain Is Not Normal” and neither are and other “Menstrual Irregularities” that women face on a daily basis. I know what you go through daily and I am out there making sure you all get heard. Let’s end the silence on this horrible disease for you, and the ones close to me whom I love, adore and care about also.
Regards
Andrew Orr
-No Stone Left Unturned
-Women’s and Men’s Health Advocate
-The Endometriosis Experts