Polycystic ovary syndrome (PCOS) is the most common endocrine/gynaecological/reproductive disorder — and most common cause of infertility — affecting 9 to 18 percent of women around the world.
Despite the prevalence of this chronic condition, one-third of women diagnosed with PCOS saw at least three health professionals over the course of two years before receiving a diagnosis, according to a study from the Perelman School of Medicine at the University of Pennsylvania.
The study, published in the Journal of Clinical Endocrinology & Metabolism, is the largest to date examining time to diagnosis, and reveals what the authors say are “major gaps” in education and support for women with the condition.
As a healthcare practitioner with a special interest in this area, I see these same issues with so many women waiting years to get a proper diagnosis and they have seen multiple healthcare professionals in both the medical and complementary medicine profession.
The signs and symptoms of PCOS are very clear and easily diagnosed, but many healthcare professionals end up focussing on one symptom, while overlooking the bigger picture and then these poor women get their condition missed.
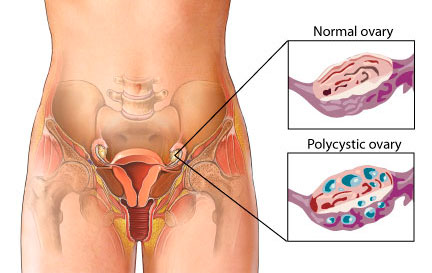
Many practitioners and public alike, do not understand the difference between PCO (Polycystic Ovaries) and PCOS (Polycystic Ovarian Syndrome) either and this creates a big issue as well. These days the two condition are actually put under the heading of the one condition, when this is not entirely true. For more information about PCO and PCOS, please click of this link (click here)
PCOS primarily affects women of reproductive age — most often between the ages of 18 to 35. The most common signs of PCOS are:
- Absent, Irregular and Inconsistent menstrual periods,
- Acne
- Excess hair growth (some women can have hair loss too)
- Central obesity
If a women presents with Acne, irregular periods, absent periods etc, there is a good chance that she may have PCOS. The problem for these women, as explained before is that healthcare providers and placing too much emphasis on only one of these symptoms, which is usually the Acne, or just that the cycle is irregular. Then women are then put on the Pill and these symptoms are masked for years, until they try and have a child and have difficulty doing so.
Women with PCOS also have an increased risk of type 2 diabetes, gestational diabetes, metabolic syndrome and anxiety and depression, and studies have shown that the longer it takes for the condition to be diagnosed, the greater the patient dissatisfaction.
These new results are concerning for those of us who do know how to deal with PCOS and other gynaecological conditions properly. These women should not be having this conditions missed. The other issue is that not only do women often wait several months or even years before care providers are able to diagnose the condition, but even after diagnosis, patients are often unsatisfied with the information and support they receive. It is such a vicious cycle.
But let’s not forget out Endo Sister’s who have endured the long road to diagnosis and management for their disease. It can often take up to 12 years for their diagnosis and again many of them have their condition missed and are dismissed. It is again such a vicious cycle of mismanagement and focus one symptoms before someone finally properly diagnoses their disease. Then many of these also complain of the management and treatment after diagnosis. We also know that many with endometriosis, also have PCOS. These two disease states can go hand in hand and both can equally be missed and dismissed.
Based on the study findings, the authors are calling for the development of international evidence-based guidelines, co-designed consumer and health professional resources and international dissemination to improve diagnosis experience, education, management and health outcomes.
Too right they should be calling for better diagnosis and better education and training for these healthcare professionals. If you don’t know how to do your job properly, or it is out of your scope of practice, get out of the way and refer these women onto people who are trained to diagnose and manage these conditions properly.
Lets, help put and end to PCOS and also put an end to Endometriosis as well. Let’s break the silence and help women get the diagnosis and care they need. Early intervention and treatment is crucial for any disease state and let’s help women get this care sooner.
Take care
Regards
Andrew Orr
-Women’s and Men’s Health Advocate
-“Period Pain IS NOT normal”
-“Leaving no Stone Left Unturned”

Journal Reference:
Melanie Gibson-Helm, Helena Teede, Andrea Dunaif, Anuja Dokras. Delayed diagnosis and a lack of information associated with dissatisfaction in women with polycystic ovary syndrome. The Journal of Clinical Endocrinology & Metabolism, 2016; jc.2016-2963 DOI: 10.1210/jc.2016-296