All to often women have gynaecological disease states “missed” and “dismissed” because their healthcare practitioner was not asking the right questions about period pain and gynaecological issues.
I didn’t know how I was going to start this post, or begin to talk about what I am about to talk about, other than I got some inspiration after a text message, and a phone call later on, from my eldest daughter some time ago.
I will talk about that soon. But let’s talk about some of the phone calls and messages I get from people every day and how some of these messages gives me a heads up into what may be going on for these people and then getting them in for a proper consult and the right help.
Every day I get phone calls, emails, Facebook messages etc, from women (young and older) who are experiencing period pain, menstrual issues, and other related symptoms and nearly all of them have the same story.
“I have been to the GP and I have had blood tests and scans and they say that there is nothing wrong”. This is what I hear all so often.
It happens so often and it is like there is a script written for these poor women who just want to get out of pain and get some sort of normal life back. I get so annoyed when I hear this repetitious line. Not at the people telling me, but knowing that these poor women really haven’t been investigated properly at all and probably won’t be unless they come and see me.
I remember I got a text that I really wasn’t expecting, as it was from my eldest daughter.
It read “Hey Dad, is endometriosis hereditary?”
To which I replied “Yes it can be, why?”
I anxiously awaited the next reply and thankfully she was asking on behalf of a friend. But this poor friend had been experiencing really bad period pain and had basically had blood tests and scans and been told that everything was normal.
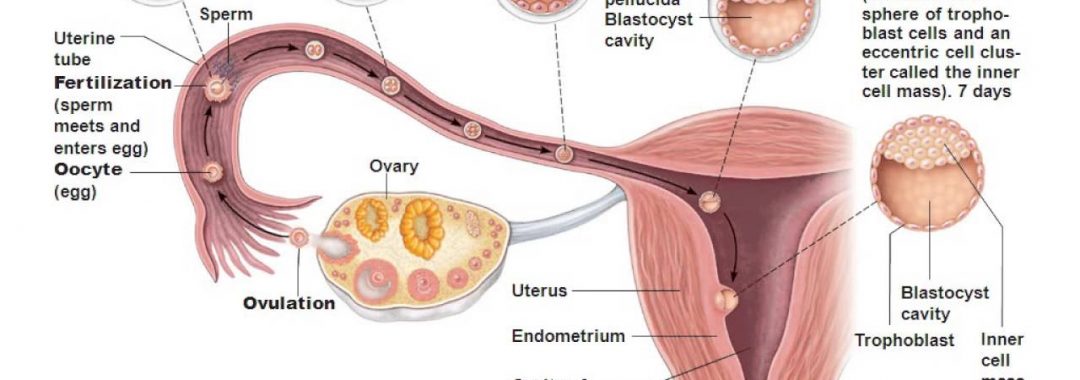
Apparently one of the scans showed some fluid in the Pouch of Douglas (POD), which can actually be a sign of endometriosis and inflammation. Worse still, this poor girl’s mother actually has endometriosis and nobody is putting two and two together and asking the question “I wonder if the daughter may have it too?”
Well, there is more than a good chance that she does have it and thank goodness my daughter actually knows the signs and knows that scans and bloods tests cannot diagnose many gynaecological issues, especially endometriosis.
Lucky my daughter also knows that you need to see an advanced trained laparoscopic surgeon who specialises in the excision of endometriosis and has done years of extra surgical training to specialise in these disease states. The good thing is that she knows that you cannot just see a regular gynaecologist to get this done.
But, not everyone is as fortunate as my daughter to know this and help her friend to come and see me to help her see my surgeon and then I can help her with management of the disease, if found (which is highly likely) after the surgery.
The other good thing is that my daughter knows there is no cure for endometriosis and that surgery isn’t going to fix the problem either. She knows it will help, and is needed, but after the surgery, the management post surgery is the most important, for disease states like endometriosis.
Unfortunately not many people know this and don’t have the disease managed properly post surgery. Women with endometriosis and some other inflammatory gynaecological issues will need a team approach, or a multimodality approach post surgery, because even with the best medical intervention, it really isn’t enough and why so many women have the disease and symptoms return, or may still be in pain and have other recurring symptoms.
There is never a one treatment, one pill, fix all approach to disease states such and endometriosis. This is where so many go wrong.
One of the main issues for women can be that they really have not seen the right healthcare professions, especially the right surgeon and unfortunately this is many of the women that have had surgical intervention. This one is so important.
Whenever I get messages from women in pain, or I consult with women who have period pain and all the other associated symptoms, there are some standard questions I ask, to know if they have been given the right information, been diagnosed properly, or seen the right surgeon.
- I always ask “what tests have you had done?” – I know that if they have only had blood tests and some scans, then these women have not been investigated, or diagnosed properly.
- Then I usually ask “Have you just seen your GP, or have you seen a specialist?”– Most of the time many women have not been referred onto a specialist and have only just been seen to by a GP. This is one of the biggest issues women face when it comes to gynaecological conditions. GP’s are just general practitioners. They are not gynaecologists and definitely not advanced trained laparoscopic surgeons. The best thing any woman can do is ask for a referral to a specialist and a good GP should know to do this anyway. This is one of the biggest reasons that women from all over the world take up to a decade to be diagnosed with disease states such as endometriosis. On a daily basis women are missed and dismissed and told there is nothing wrong, go on the pill, or that they have some inflammatory bowel condition, when in fact they have endometriosis, or adenomyosis, or some inflammatory gynaecological issue. Btw, this isn’t to put GP’s down, unfortunately this is what happens to so many women and why it often takes up to a decade for women to be diagnosed with diseases such as endometriosis. This is an unfortunate fact and it needs to change.
- Then I ask “Have you had a laparoscopy?”– One of the most common responses is “What is a laparoscopy?” and that way I know they haven’t had one done. A laparoscopy is the gold standard investigation of the pelvis and the only way to properly diagnose disease states and causes of period pain, such as endometriosis.
- If the woman has had surgery I then ask “was the surgery done publically, or privately?” – This will tell me a few things. It will let me know if it was just done be a public surgeon, who probably isn’t an advanced trained laparoscopic surgeon. The issue is that there really aren’t that many advanced trained laparoscopic surgeons that do public work, and even if you strike the jackpot and do happen to get one, there is a good chance they are only in a teaching role to instruct a trainee surgeon to do the surgery anyway. But mostly women do not get an advanced trained laparoscopic surgeon in the public system. It is sad, but true unfortunately. Many times the first surgery in the public sector is purely investigative too and no excision (disease removal) is performed. This means that the woman has to come back for further surgery, or surgeries.
- If they the woman has had surgery done previously by a private specialist then I usually ask “Who was the surgeon that did your investigation and surgical procedure?” – Sometimes I can ask if the surgeon was an advanced trained laparoscopic surgeon and the patient usually will respond to not knowing, or even know what I was talking about. That usually gives me a clue that it most probably wasn’t, but then I can go and check the specialists qualifications online and see if they are, or most probably aren’t, an advanced trained laparoscopic surgeon who has done years of extra specialised surgical training.
All those 5 questions can tell me much about what some of these poor women have had done, or haven’t had done, and then I can formulate an appropriate treatment plan and management for these women moving forward.
It is always hard explaining to the ones that have had surgery before that they haven’t seen the right surgeon and that they are going to need further surgery. The hardest thing for me is seeing women on support pages about to have their first surgery and I always worry that they aren’t seeing the right surgeon and if they don’t, there is a good chance that they are still going to be going through the same issues, over and over again, until they find the right person to help them.
If only I could see all these women before they did anything, so that they can be given the right information and the facts and be managed properly.
The good thing is that when I do get to see women who chose to see me, I can explain to them the facts and the right information and then why and how with a proper surgeon, that it can make a huge difference to how they are feeling and their recovery and management post surgery.
I can also explain how surgery really is necessary, but is only a small part of their overall treatment and management of their disease moving forward. I can also explain the facts around their disease moving forward too and make sure that women under my care are given the right information, the right investigations and right management going forward.
This is why my initial consultations take about an hour and a half and we go over everything from their health history, medical history, hereditary issues, diet, lifestyle, surgical intervention, medications, natural medicines, blood tests, scans, investigations, sleep, sexual health, libido and everything that a woman needs to know about her particular issues.
It is also about listening to a woman’s concerns and complaints and really hearing what she has to say and is experiencing.
Then I formulate a treatment plan and management and 20 page report of findings for them for what we are going to be doing to help them moving forward.
I also give them a step by step treatment plan of treatments and medicines etc they will need too. That is why my motto is “No Stone Left Unturned”, because there is no stone left unturned and I also make sure they see the right people (surgeons and anyone else that they may need to see).
If there are things that I can’t do (surgery etc), I make sure that my patients only see the best people, in my trusted network, and then I can help manage their disease state alongside other specialists and medical interventions.
I wish I could see every woman before they went for any investigation, or surgery, so I can point them in the right direction and help them manage their gynaecological condition properly.
This is why I am so passionate about doing my posts on social media, or giving time for charity events to talk about women’s health issues and gynaecological issues such as endometriosis, adenomyosis and PCOS.
It is why I do healthcare practitioner education and seminars to help educate them better too, so that they can help their patients better and not miss and dismiss them.
I just hope that I can help those who have not been heard and that have been missed and dismissed. I also hope we can get people to listen to the things I have presented above and also help women get a voice, be heard and get government listening and get more education to younger women too.
Lastly, I cannot say it often enough….. Period Pain “IS NOT” normal and if you, or your daughter, or your sister, or your mother, or cousin, your best friend, or anyone you know has period pain, especially bad period pain and other symptoms, please, please, do not tell them that this is normal.
Period Pain is not normal and women who are experiencing period pain need to see someone who specialises in women’s health and gynaecological conditions, so that they can be investigated properly and have their issues managed properly too.
If you do need assistance with a women’s health issue, you can make a booking to have a consultation with me. Please call my friendly staff to find out more.
Regards
Andrew Orr
-No Stone Left Unturned
-Women’s and Men’s Health Care Advocate
-The Endometriosis Experts
-The Women’s Health Experts