One of the things I teach my patients is the importance of properly restoring the microbiome for optimum health and also reducing inflammation in the body.
Many people’s daily bloating, fluid retention, gastrointestinal symptoms, health issues, chronic disease states are being exacerbated by an unhealthy balance in this unique ecosystem we call the microbiome.
The problem is that many people do not really understand the importance of the microbiome, and even many healthcare professionals do not fully understand how to help with proper microbiome repair and restore.
Many people are also led to believe that by just taking probiotics, that this is enough to restore the healthy bacteria in the gut/microbiome.
I wish it was that easy, but it isn’t and this is why many people continue to have gastrointestinal issues, inflammation and chronic health issues, despite thinking that are doing the right thing for their gut health.
What is the Microbiome?
The human gastrointestinal tract (GIT) is host to an extraordinary amount of microorganisms composed of bacteria, viruses and microbes, collectively known as the microbiome. The microbiome is the name given to all of the genes inside these microbial cells.
Every human being has anywhere between 10 trillion and 100 trillion microbial cells all working together in a symbiotic relationship. This benefits both the microbes and their hosts, as long as the body is in a healthy state.
Recent scientific advances in genetics mean that humans know a lot more about the microbes in the body. There has been lot of time and money put into researching the interactions within the human body’s ecosystem and their relevance to health and disease.
The two terms ‘microbiota’ and ‘microbiome’ are often used to mean the same thing and are used interchangeably. I will explain the differences between them and how both are being used and researched in modern medicine.
You exist in a symbiotic relationship with your bacterial ecosystem, and there is a two-way relationship that makes your health inseparable from that of your microbiome and vice versa.
The benefits of a healthy microbiome/microbiota
The benefits of a healthy microbiome/microbiota, extend beyond the gut and digestive system and has a significant systemic impact on some the following:
- Nutrient metabolism
- Body composition (weight)
- Cardiovascular health,
- Chronic disease states
- Inflammation in the body
- Pain pathways
- Immunity
- Mental Health
- Neuroendocrine function
- Gene Expression
What is the Microbiota
The gut microbiota used to be called the microflora of the gut. The importance of the microbiota has been known for a long time, but now medical science is discovering just how important it is, and it is now becoming a cornerstone of preventive medicine.
The gut microbiota contains over 3 million genes, making it 150 times more genetically varied than the human body. The gut microbiota of each individual is very unique and it has a major contribution to how a person fights disease, digests food, and even his or her mood and psychological processes.
This symbiotic relationship greatly benefits humans. The presence of this normal flora includes microorganisms that are so present in the environment that they can be found in practically all animals from the same habitat.
However, while there are good bacteria found within these native microbes, some of these microbes also include harmful bacteria that can overcome the body’s defences that separate them from vital systems and organs. There are beneficial bacteria in the gut, and there are harmful bacteria that can cross into wider systems and can cause local infections of the GI tract. These infections can then cause infection and inflammation and can also worsen disease states in the body.
What is dybiosis?
The microbiome plays an important role in resisting intestinal overgrowth of externally introduced populations that would otherwise cause disease. In our microbiome, the “good” bacteria compete with the “bad,” with some even releasing anti-inflammatory compounds.
Bacterial dysbiosis produces an endotoxin called lipopolysaccharide (LPS). It is one of the most inflammatory substances known. LPS is also major contributor to the inflammation, which then drives many chronic health conditions and disease states.
These bad bacteria are called dysbiotic bacteria and cause a process called ‘dysbiosis’.
Broadly speaking, dysbiosis indicates the existence of either the wrong microbiota (e.g. overgrowth of bacteria, fungi and/or parasites) and/or the wrong numbers of the right microbiota (imbalances in composition), or either, in the wrong place.
Dysbiosis causes increased gut and intestinal permeability, which can lead to what we call leaky gut, or leaky gut syndrome. Dysbiosis can also consequent lead to up-regulation of inflammatory pathways and lead to increased inflammation in the body.
Dybiosis is implicated in many chronic diseases
Dysbiosis is very common it the western culture and bacterial dysbiosis is now being linked to causing, or exacerbating many health conditions and disease states. Research has found links between bacterial populations, whether normal or disturbed, and the following diseases:
- Endometriosis
- Adenomyosis
- PCOS
- Asthma
- Autism
- Auto-immune conditions
- Cancer
- Celiac disease
- Colitis
- Inflammatory Bowel Disease
- IBS
- Crohn’s Disease
- Diabetes
- Eczema
- Heart disease
- Malnutrition
- Multiple sclerosis
- Arthritis
- Obesity
- Metabolic Syndrome
What Causes Dysbiosis?
There are many things that lead to bacterial overgrowth, which then leads to dysbiosis. This is why many people suffer bloating, reflux, nausea, constipation, inflammatory bowel symptoms, and many other gastrointestinal symptoms daily.
Day-to-day risk factors include a western-based diet, overly hygienic living (being too sterile), alcohol, certain medications, hormones and the use of antibiotics.
Mood disorders, stress and being overly busy are also a big factors with creating dysbiosis and something that many overlook, or do not even realise. Yes, stress is a big factor in many gastrointestinal symptoms people experience daily.
With all these factors it means that almost everyone will have some degree of dysbiosis at some point in their life.
Many constantly have dysbiosis and why they often have long-standing digestive symptoms such persistent pain and bloating, constipation, alternating diarrhoea or other digestive imbalances. We also commonly see this with endometriosis and the dreaded “endo belly”
Medications Cause Dysbiosis and Significantly Affect The Microbiome
As mention already, many medications and hormones actually have a toxic affect on the microbiome and can cause dysbiosis. It is crucial to for all of us to understand the consequences of medication use in the gut microbiome. I’ll talk about this in my next post.
The good news, however, is although medications can cause a dysfunctional microbiome quite rapidly, you can begin to restore a healthy microbiome just as quickly through strategic microbiome restore.
Proper Microbiome Restore Protocols
When it comes to proper microbiome restore, it isn’t just as easy as taking any old probiotic, or a combination of probiotics. Microbiome restore requires and individualised and strain specific approach and it needs to be done in stages with antimicrobials, gut repair and prebiotics as well. Dysbiotic microbes can be hard to treat effectively because they have evolved and adapted to life inside human beings. Consequently, elimination of these organisms requires a similarly evolved and adapted approach. This is all part of the microbiome restore protocol I use with my patients.
A New Understanding
When it comes to the perfect microbiome, researchers have discovered there is no ‘one size fits all’ across various populations. It is important to recognise that not all strains are created equal when it comes to their ability to rebuild a healthy microbiome.
What is now known is that there are only certain types of good probiotic bacteria that have benefit for our gut and microbiome, and that some strains of probiotic bacteria have no benefit. These new finding mean that we need to adopt a strain specific approach when repairing and restoring the microbiome.
From recent investigations and research, the best results are gained by introducing strain specific influential probiotic that have beneficial functions. These specifically influential strains are able to restore each patient’s unique microbiome by promoting the growth of key commensal (symbiotic) groups, but also by improving overall GIT function.
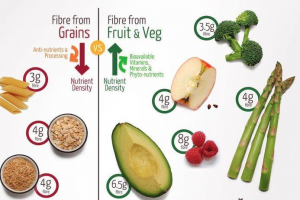
The Importance of Prebiotics
In addition to prescribing a specific probiotic formulation, prebiotic therapy is needed to help support and encourage the establishment of healthy microbiota by significantly increasing the numbers of beneficial bacteria. Without prebiotics, the probiotic bacteria do not grow and this is why they are essential for microbiome restore. Prebiotics are not talked about enough and many people do not realise their importance and often wonder why their probiotics are not working effectively enough.
Prebiotics are also needed to promote the growth of healthy microbiota, begin refurbishment of gut mucosa and improve gastrointestinal immunity. Prebiotics also help with inflammation and also support the integrity of the intestinal barrier, provide healthy immune responses and promote intestinal microbiome balance.
Microbiome Restore Protocols
With emerging research now highlighting the significance of developing and maintaining a healthy microbiome, it is important that everyone knows the importance of appropriate probiotic and prebiotic combinations. By supporting the restoration and repair of our micriobiome, we can all optimise our health, improve treatment outcomes and also help with reducing the risk of many chronic disease states.
If you would like to find out how to restore your microbiome properly, please give my friendly staff a call and find out how I may be able to assist you. Online and in person consultations are available. Some conditions apply.
Regards
Andrew Orr
-No Stone Left Unturned
-Women’s and Men’s Health Advocate
References
-
Walker A, et al. Phylogeny, culturing, and metagenomics of the human gut microbiota. Trends Microbiol. 2014;22:267–74.
-
Collado MC, et al. Role of commercial probiotic strains against human pathogen adhesion to intestinal mucus. Lett Appl Microbiol. 2007;45(4):454-60.
-
Leahy SC, et al. Getting better with bifidobacteria. J Appl Microbiol. 2005;98(6):1303-15.
-
McFarland LV. Systematic review and meta-analysis of Saccharomyces boulardii in adult patients. World J Gastroenterol. 2010;16(18):2202-22.
-
Jahn HU, et al. Immunological and trophical effects of Saccharomyces boulardii on the small intestine in healthy human volunteers. Digestion. 1996;57(2):95-104.
-
Jahn HU, et al. Immunological and trophical effects of Saccharomyces boulardii on the small intestine in healthy human volunteers. Digestion. 1996;57(2):95-104.
-
Dahan S, et al. Saccharomyces boulardii interferes with enterohemorrhagic Escherichia coli induced signaling pathways in T84 cells. Infect Immun. 2003;71:766-773.
-
Hsieh H. Versalovic J. The human microbiome and probiotics: Implications for pediatrics. Curr Probl Pediatr Adolesc Health Care. 2008;38(10):309–327.
-
Lam EK, et al. Enhancement of gastric mucosal integrity by Lactobacillus rhamnosus GG. Life Sci. 2007;80(23):2128-36.
-
Seth A, et al. Probiotics ameliorate the hydrogen peroxide-induced epithelial barrier disruption by a PKC- and MAP kinase-dependent mechanism. Am J Physiol Gastrointest Liver Physiol. 2008;294(4):G1060-9.
-
Gibson GR. Roberford M. Dietary modulation of the human colonic microbiota: introducing the concept of prebiotics. J Nutr. 1995;125:1401-1412.
-
Fastinger ND, et al. A novel resistant maltodextrin alters gastrointestinal tolerance factors, fecal characteristics, and fecal microbiota in healthy adult humans. J Am Coll Nutr. 2008;27(2):356-66.
-
Raninen K, et al. Dietary fiber type reflects physiological functionality: comparison of grain fiber, inulin, and polydextrose. Nutr Rev. 2011;69(1):9-21.
-
Robison LE. Reeves S. EpiCor® and its immune effects on gut health. Embria Health Sciences, LLC. [Online]. No date. Available from: http://www.embriahealth.com/upload/pdf/EpiCor%20Science%20%20EpiCor%20and%20its%20Immune%20Effects%20on%20Gut%20Health_FINAL.pdf [Cited 16/02/13].
-
Jensen GS, et al. Antioxidant bioavailability and rapid immune-modulating effects after consumption of a single acute dose of a high-metabolite yeast immunogen: results of a placebo-controlled double-blinded crossover pilot study. J Med Food. 2011 Sep;14(9):1002-10.
-
Bartoli, C., Frachon, L., Barret, M., Huard-Chauveau, C., Mayjonade, B., Zanchetta, C., … & Roux, F. (2018, May 30). In situ relationships between microbiota and potential pathobiota in Arabidopsis thaliana. The ISME Journal. Retrieved from https://www.nature.com/articles/s41396-018-0152-7#article-info
-
-
-
Clapp, M., Aurora, N., Herrera, L., Bhatia, M., Wilen, E., & Wakefield, S. (2017, September 15). Gut microbiota’s effect on mental health: The gut-brain axis. Clinics and Practice, 7(4), 987. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5641835/
-
NIH Human Microbiome Project. (n.d.). Retrieved from https://hmpdacc.org/
-
Shepherd, E. S., DeLoache, W. C., Pruss, K. M., Whitaker, W. R., & Sonnenburg, J. L. (2018, May 9). An exclusive metabolic niche enables strain engraftment in the gut microbiota [abstract]. Nature, 557, 434-438. Retrieved from https://www.nature.com/articles/s41586-018-0092-4
-
The Human Microbiome Project Consortium. (2012, 14 June). Structure, function and diversity of the healthy human microbiome. Nature, 486, 207-214. Retrieved from https://www.nature.com/articles/nature11234
-
Ursell, L. K., Metcalf, L., K., Wegener Parfry, L., Knight, R. (2012, August). Defining the human microbiome. Nutrition Reviews, 70(Suppl 1), S38-S44. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3426293/