Sex is something that nearly every human on this planet gets to experience, and for each person, the experience of sex can be different. Many people have different perceptions on this important topic, so lets talk about sex, how often, what’s normal and how to boost that libido in those having issues.
As a healthcare practitioner who is a Master in Women’s Health Medicine and a Master of Reproductive medicine, I have to talk about the topic of sex on a daily basis. A lot of people come into my clinic (both men and women) with varying expectations and thoughts on what is normal, when concerning sex. Unfortunately a lot of people are way off the mark when it comes to a healthy sex life and what a healthy libido should be.
Libido is influenced by our health
If you do not have a healthy libido, there could be something wrong with your health. Yes, what you eat, think, do etc, all plays a part in your sexual appetite. But, we can all have differing libido’s and it is important to understand this and seek help if you are having issues. A healthy libido is a sign of a health body and healthy mind.
What defines a healthy sex life
The average healthy human being in a healthy relationship should be having sex at least 1-3 times per week, depending on age etc. I know a lot of you are lucky to be having sex 3 times per month.
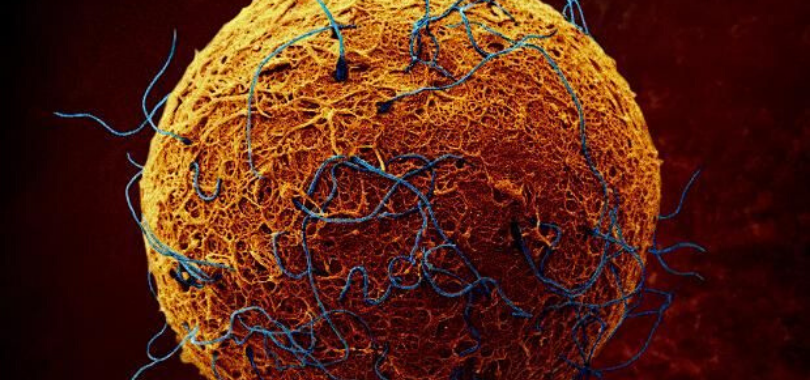
What’s concerning about this is, some of these people are trying to have a baby and can’t understand why they aren’t falling pregnant. The answer is obvious, but, I’ll say it anyway, you have to have sex regularly to fall pregnant and it has to be at the right time. You need to be trying every day, or every second day of your cycle as we now know ovulation just doesn’t take place mid-cycle only.
Clinical research shows that more than 70% of people are ovulating before day 10 and after day 17 of their cycle. So if you are just trying it that small window of day 10-16, this could be the reason you aren’t falling. Btw, don’t stop having sex just because you are doing IVF. Sex (climax in particular) helps with implantation so stopping having sex is only hindering your chances of conception. I have talked about this is a previous post (click here to read)
We also now know that sperm also play a part in a health menstrual cycle as they help to trigger certain hormones to trigger ovulation and thus help with regulation of the menstrual cycle. It may explain why women using barrier methods of contraception have more issues with irregular cycles and menstrual issues. Not that we are promoting unsafe sex mind you. This is for couples in a healthy relationship. I have spoken about this is a previous post too (click here to read)
Why is climax/orgasm so important
Climax also stimulates blood flow into the uterus; helps trigger certain hormones and also helps with implantation. Climax also helps ones libido and it can even help in the treatment of depression.
We also hear the jokes about men and their ever-constant desire to have sex, but most of the time this is greatly exaggerated. In practice I am actually seeing that women are now the ones with the higher libidos and it is the men that are having all the problems. Stress is a big factor these days. We are also seeing many men with testosterone deficiency. Being overweight and unhealthy physically and mentally can be a factor also.
It has also been shown that regular sex, even if scheduled, actually helps with the libido and helps with the desire around wanting more sex.
Understanding differing libido’s
Men and women are different when it comes to libido and the desire around sex. Men need to understand that it can often take all day for a woman to arouse her desire around wanting sex. Men need to know that women need to be wooed, given playful thoughts, mind play and a place to feel safe to get her into the mood for sex. Guys, apparently helping out around the house also helps (hint, hint)
Intimacy is more than just sex
Remember sex is a healthy part of a relationship and a healthy libido shows good health. Sex is also a way of connecting with your partner and couples should find way to prioritise each other so that this connection happens regularly. It is also about intimacy and that sacred intimacy, which is on a whole other level to the physical act of just having sexual intercourse.
What affects a libido?
Many people do talk about having differing libido’s, or having trouble with libido, and it is important to understand what may be affecting ones sex drive.
So, what are some of the main things that effect libido?
- The Pill – First and foremost, the pill for women. Anything that decreases fertility can decrease your sexual desire. The pill also turns off certain receptors responsible for conception, which can then turn off the libido.
- Stress – Constant low grade, or high grade stress, is a big problem when it comes to loss of libido. It can cause impotence & erectile dysfunction in men and loss of libido and menopausal symptoms in women.
- Medications – Drugs such as anti-depressants, the pill, anti-inflammatories, and lots of other medications can ruin your sex life. They can also delay or stop orgasm. There are some that can improve it too. Not many!
- Alcohol and recreational drugs– This one is pretty self explanatory. We’ve all heard the saying ‘Fosters flop’ from drinking too much beer. Drugs such as marijuana, speed, and other illicit drugs can all impair libido
- Sexual Abuse– A history of sexual abuse can definitely affect the sex life. This needs to be dealt with by speaking to a counsellor, psychologist or sex therapist.
- Health Problems– Health problems such as Low Thyroid, Diabetes, being overweight, depression, eating disorders, can interfere with your libido and sex life.
- STD’s– Some STD’s are often undetected and cause pain and discomfort during sex, which leads to not wanting to have sex. Many of these can be cleared up with medication so that your sex life can return to normal. Some STD’s are there for life but can be controlled. STD’s such as herpes and HIV don’t have to stop your sex life.
- Gynaecological issues – Some gynaecological disease states such as Endometriosis and Adenomyosis can make sex painful and cause a lack of desire. Have a read of my article about painful sex. Women with PCOS can have low libido as a result of hormonal fluctuations and insulin resistance.
- Diet– This is a big one. If you eat the wrong foods the body will respond accordingly. Your sex life can be ruined by what you put in your mouth to sustain your body.
- Exercise– Over-exercising can stop you getting a period and cause fertility issues in both men and women. Reduce the exercise and the libido will respond accordingly. Exercise can also increase libido. It is about moderation.
Final Word
If you are having trouble with your libido there are many medical and natural products that have been shown to assist with low libido and help with a healthy sex life for both men and women. It is important that you talk to a qualified healthcare practitioner about issues to do with sex and libido. You need to see an expert who is trained to know issues that may be causing your particular issues. The can also give you dietary and lifestyle advice to help in this area too.
If you do need help with issues around sex and libido, please give my friendly staff and call and find out how I can assist you. I also have a great network of sex therapists, psychologists and medical specialists I work in with as well.
Regards
Andrew Orr
-No Stone Left Unturned
-Master of Women’s Health Medicine
-Master of Reproductive Medicine
-The Women’s Health Experts