Every day I hear stories about women being told their symptoms are normal, or they have been missed and dismissed for many years. Some of the things I hear women get told gets me angry sometimes.
Many of you have also been told utter BS (bullshit… sorry for swearing) and it just gets me so upset to hear this BS continues in both the public arena, closed groups and by other healthcare professionals. When are women going to get the support they need and get the health system to start listening?
When I have to talk to men about this topic, usually partners of women who have endometriosis, or who suffer bad period pain and other symptoms, I explain it like this. I explaint that if guys had pain in their testicles daily and couldn’t walk, were curled up on the bedroom floor, had vomiting from the pain, had to ingest copious amounts of pain killers etc to just function, then governments would rewrite the health system, laws would be made, research would be done and those testicles would endure pain no longer. Well.. that is what I think anyway.
The biggest problem for women is that many of you believe that period pain is normal, because that is what you have been led to believe. Then some healthcare professionals reinforce it and you are basically made out to be neurotic when you try and tell anyone that you can’t handle it any longer.
Suck it up they say. Take some painkillers they say. Have a baby they say. Take the pill they say. There are so many BS things said to you all and all of them are wrong. There are so many other things wrong with everything from support groups sprouting misinformation, GP’s telling people misinformation, specialists telling people misinformation and people now relying on “Dr Google” as the gospel for their healthcare diagnosis. This is where the problem all starts and in many ways ends.
So how do we fix this?
Well, education is the first step. This is not just to the public, but to healthcare professionals as well. We also need to start educating women at a young age that “Period Pain IS NOT normal” and neither are other menstrual irregularities that could be the signs of other gynaecological conditions.
Early intervention and treatments and management it always going to be the key to any disease state. Thousands of years ago in China, the Yellow Emperor had a classic saying “To treat a disease once it has already started and been expressed in to the body is like trying to forge arms once a war has already started, or trying to dig a well once one if already thirsty”.
Trying to treat any disease once it has been expressed is hard work and for some diseases, nearly impossible. Prevention is the key and like any disease, we need to find ways of preventing endometriosis too. But if the disease is expressed, we need proper education to know the signs, know the symptoms and get early intervention and treatments and management as soon as possible.
Endometriosis can be managed, just like any other disease. I have asthma and I am symptom free because I manage it properly and have the training and education and proper treatments to manage it. I still have the disease, but I have learnt to manage it and be symptom free most of the time. Doesn’t mean I don’t get the odd flare though.
The same can be for endometriosis if you see the right people and get the right treatment and health management. Let’s be real about this, even with the best management, sometimes you will still just have a bad day, or a few bad days, despite what you do. This is the reality of living in chronic disease state.
Finding the right people to listen and to do the right investigations and management can be hard and we also need people to listen and do the treatment too. We do need people to take some ownership in their health too. I mean this is a caring way when I say this.
Having had a debilitating and life threatening disease I know how hard it can be just to function, both physically and emotionally. I also know hard it was for me to find the right people to help me too. So I get it. But we still need to talk about this and be honest about ownership too.
Please don’t buy into the diagnosis and the label if you know what I mean. Doing that can eat you up, make you angry/mad and then makes things worse. I know because I have been there. I now teach people to rise up, ditch the label and be the best they can be daily. But, it can be hard work, as many of you know. I get it.
So, lets start with looking at the facts around Endometriosis first and in the next lots of posts I’ll talk about the management and treatments to get women their lives back
The Facts about Endometriosis
1. Period Pain IS NOT Normal- You are not meant to get period pain. Some slight heaviness, or mild discomfort maybe, but pain you should not get at all. Pain is not normal and we need to stop saying it is.
2. A significant portion of women with Endometriosis are asymptomatic– A significant portion of women DO NOT get pain, or any symptoms at all. Just because you do not have pain, does not mean you do not have endometriosis.
3. Symptoms DO NOT correlate to the extent of the disease– As mentioned previously, some women with relatively small amounts of endometriosis will have significant pain, have lots of symptoms, while some women who are riddled with it may have no symptoms at all. This is why i do not like the staging system (1-4) because it really does not accurately describe a women’s symptoms, or have it correlate to the extent of the disease.
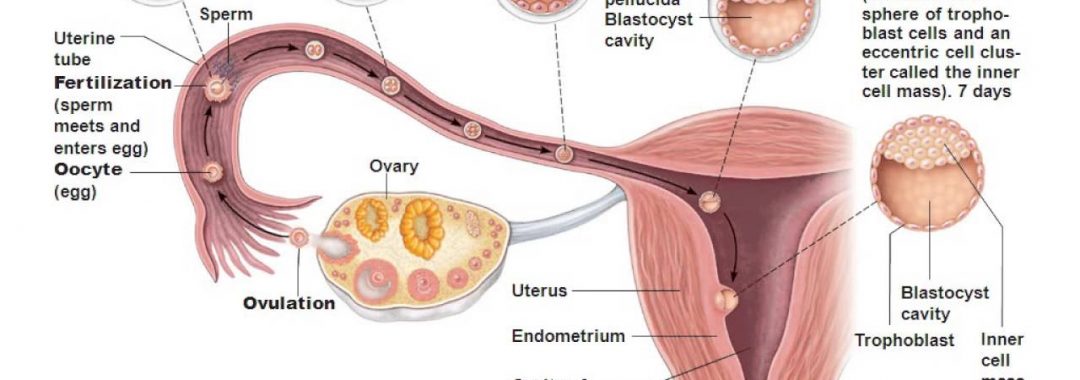
4. The only way to diagnose Endometriosis definitely is via surgical intervention– Scans, blood tests etc do not diagnose endometriosis. You cannot have a scan to diagnose endometriosis and you cannot have a blood test to diagnose endometriosis.
The definitive diagnose IS and ALWAYS WILL BE via a laparoscopy/laparotomy, along with a biopsy and tissue taken to examine. A laparoscopy is the goal standard investigation of examining the pelvis and for investigating gynaecological disorders such as endometriosis.
The laparoscopy also need to be done by what we call an Advanced Trained Laparoscopic Surgeon, who has extra years of surgical training, and who specialises in this disease and specialises in the excision of endometriosis. It can’t just be done by a regular gynaecologist and this is where many go wrong. They just haven’t seen the right surgeon first up who has the proper skills to deal with it effectively. Many women have been under-serviced surgically previously and this is a big issue. It just means that they may get some relief, but it will not be long lasting.
The first surgery should always be your best surgery and early intervention and management of this disease is crucial. The longer it is there, the worse it can become. But, please know that surgery does not cure endometriosis. It is just the first stage in the management of the disease and endometriosis needs ongoing care and a multimodality approach to treat if effectively. It needs a team to manage it properly.
5. There is NO cure for Endometriosis– At present there is no cure for endometriosis. Just as I mention my asthma before and it having no cure, the same applies to endometriosis. Once it is expressed into the body, it will always be there. Even if someone becomes asymptomatic, the disease it still there. But while there is no cure, the disease can be managed and women can become asymptomatic with the right help, right treatments and right management. I see this is practice daily.
6. Having a baby will not cure endometriosis– Many women are told to go away and fall pregnant and have a baby as this will fix their period pain and cure their endometriosis. This is a load of rubbish. Having a baby will not cure endometriosis. It may stop you having period pain for 9-10 months because you won’t be getting your menses, but you can still get other symptomatic pains and referral pains etc. Pregnancy does not fix endometriosis. The reason why women are told to go and have a family as soon as possible is because endometriosis can make it harder to fall pregnant, for some people.
7. Endometriosis may cause Infertility– While it may make it hard to fall pregnant for some women, other women with it may have no trouble falling at all. But women do need to be educated that it could affect your fertility and one of the major reasons women end up seeking help for fertility services.
8. Endometriosis is Estrogen Driven, Not caused by Estrogen dominance– Estrogens do drive endometriosis. This could be from oestrogen’s in our diet, in our environment, from hormones, drugs, plastics, abdominal fats, body fats and any small amounts of circulating oestrogen’s. Estrogens do not have to be in excess, or be dominant to drive endometriosis.
9. The Pill, or Contraceptives DO NOT fix endometriosis– While the pill and contraceptives can help with hormonal regulate and in some cases even stop the period, they do not fix endometriosis. In many cases the Combined pill can actually make it worse because of the oestrogen’s in it. Plus it then masks the symptoms of endometriosis and then when a woman comes off it, the endo is still there and for some women it could lead to them being infertile. The pill masks endometriosis and many other gynaecological issues. It does not fix them
10. You can have Endometriosis at a Young, or Older Age– Endometriosis does not discriminate age. Young girls can have it and older ladies can have it also. It can present at almost any age once the menses has started and can continue even when the menses has stopped. The symptoms may get less with menopause though.
11. Hysterectomy does not cure endometriosis– Hysterectomy does not fix endometriosis because many times endometriosis is not in, or on, the uterus and it can present anywhere in the body. It has been found in the joints, in the brain, around the heart, on the retina of the eyes, around the bowel and in nearly every part of the body. So removing the uterus does not cure endometriosis in many cases.
12. Endometriosis requires a multi modality approach– Like many diseases we all face, there is never one particular miracle cure, or miracle treatment for endometriosis. It requires a multi modality approach to manage it properly. This is how you diagnose, treat and manage endometriosis properly
13. Endometriosis IS NOT an autoimmune disease– Endometriosis is not an autoimmune disease. It is an autoimmune like disease because it is made worse by inflammation in the body, but it cannot be classed as an autoimmune disease.
14. There Are Hereditary and Genetic links– While we do not know the exact cause of endometeriosis, we do know that it does run in families and it there is genetic and hereditary links.
15. Endometriosis can cause many other issues in the body– Like any inflammatory disease, endometriosis can cause issues with moods, interfere with hormones, disturb sleep, cause fatigue, cause depression, exacerbate mood disorders, cause muscular pain, cause skeletal pain, have pain refer down your legs, make your joints ache, cause bowel movements to be difficult, cause loose bowels and IBS like symptoms, cause UTI like symptoms, cause bladder pain, nocturnal urination, pain with sex, pain and bleeding with exercise, ovulation pain and so many other symptoms not mentioned.
It can cause many issues both physically and emotionally and people need to be aware of this. Some women are at the point of suicide and recently we have seen women take their lives, because they just have not been listened to and it has all become too much.
There is probably a few more things I need to add in here. Please feel free to add comments to add in more. But, this is a start and hopefully people can learn from this and we can start educating people on the facts around this horrible disease. Please know there is always help.
Please know the disease can be managed with the right people on board helping you. Please know there are some really good support groups out there too.
Please know there are some amazing women ( and some men) out there trying to be your voice and get people to listen. Hopefully one day we will get a cure and women will get the treatment and management of this disease that they so desperately deserve. Sorry for the long post. But we need to get this out there.
Take care amazing people. Keep your chins up and know that there are people who will listen too.
If you would like to book in a consultation with me, please call my friendly staff, or using the automated emails system on the website.
Let me hold your hand and care for you and assist you in every step of the way to better health and a better way to live daily.
Regards
Andrew Orr
-No Stone Left Unturned
-Women’s and Men’s Health Advocate
-Period Pain is not normal