It is now known that modern day busyness, stress, anxiety and depression can significantly impact a couples chances of conceiving. When helping couples with fertility and achieving a pregnancy, one of the biggest issues I see overlooked is a couple’s emotional health. During the assessment of anyone’s fertility, depression, anxiety and stress scores (DASS) should be taken into consideration. Other assessment methods to look at anxiety and heightened adrenalin should also be utilised. It is so important to touch base on the topic of emotional health and make couples (or those who are single) aware of emotional factors that may be affecting their chances of conceiving.
I always recommend seeing a counsellor/psychologist
I always recommend that everyone should check in regularly with a counsellor/psychologist, but less than 10% of people do. What many do not realise is that their underlying stress, anxiety and other emotional concerns are actually a big part of them not being able to conceive, and that looking after our emotional health is just as important as looking after our physical health. There is research to suggest that a parent’s emotional state can be passed onto a child via the sperm, eggs and the parental mode of inheritance. Everything we put in our body, physically and emotionally, can be passed on to the unborn child. This is crucial to understand before considering having children because at the end of the day, it could affect them greatly.
Identifying the impacts of busyness, stress and anxiety
Another common observation I see when people are trying to conceive is they are adamant that they are not stressed, yet their mood/stress scores say otherwise. Many people have normalised their busyness and running on high levels of adrenaline to the point where they do not equate their heightened emotional states as being stress or anxiety. From an outside perspective, I can physically see how anxious and stressed some people are, but it is often hard for people to self-reflect and understand their emotional state.
Control issues exacerbating anxiety and stress levels
Statistically speaking, women have a higher likelihood of being the driving force behind wanting a baby/family so it is easy to see why they may be more focussed or driven in this regard. This also means that they carry a lot of the stress that comes with that. Unfortunately it is becoming more common to see said people struggle with letting go of control and feeling out of control which leads to underlying stress and anxiety. Occasionally this too leads to stress and instability in their relationships, especially if their partner isn’t stepping up.
The one thing I try to explain to all couples is that when it comes to IVF or assisted reproduction, nobody is in control. Everything is timed and controlled by hormones and medications and nobody can control that. Trying to control everything leads to high stress levels, activated adrenalin, heightened anxiety, and a vicious cycle of feeling like more control is needed. The only thing people can control is what they put in their mouths (food, medications, and supplements), how much they exercise, and how well they care for their emotional health. That is it.
Making the changes you need to do now
So many people try to justify their actions and behaviours with statements such as, “I will slow down and make time for myself once I am pregnant, or once I have the baby.” Any parent will tell you that once a child is born, there is hardly any time for yourself and things get a lot busier. The reality is that you need to work on yourself now, while you have the chance. It is not only important for you, but also for your child.
One of the things I say to future parents is this: “If I gave you your baby right now, what would you have to do to ensure its survival and yours? What changes in your life would you have to make?”
I then let them sit and think carefully about it because in reality, it would mean many changes to one’s life. The honest truth is that despite change often being uncomfortable, changing your life is exactly what you have to do right now to create the baby as well. I also tell parents that if you don’t have time for yourself, to do self-care, or to work on yourself, then you really need to question if you have time to have a child too. I don’t mean this in a bad way. I say it with absolute care and understanding of how demanding life gets when one is a parent.
Counselling needs to be mandatory
This is why it is so important to do counselling whether you are going through IVF or trying to conceive naturally. It is my personal belief that for the benefit of the parent/s and the child, counselling should be mandatory as many issues of not falling pregnant actually stem from high stress levels, anxiety, adrenaline, and an inability to slow down. It all stems back to control, and then lack of control, which then creates anxiety and stress. There can also be relationship dynamic issues that need to be addressed prior to having a baby. All this and more is not a good recipe to make a baby, or achieve a successful pregnancy outcome.
Stress animals don’t conceive and it applies to humans as well
The one thing we know from basic biology is that stressed animals do not conceive or will not carry a pregnancy. Many of our breakthroughs in fertility medicine actually come from vet science, where animals have undergone IVF or forms of assisted reproduction. We often forget as humans, that we too really are just animals.
Numerous studies have indicated how anxiety, stress and heightened adrenaline (common states of existence for many people) have a detrimental effect on egg quality, sperm quality, embryo quality, implantation, and overall pregnancy rates.
How busyness, stress and anxiety affect fertility and pregnancy outcomes
Going through IVF, or just trying to fall pregnant, is often described as the most stressful event in the lives of some couples. This is even more heightened if there are difficulties in achieving a pregnancy. There is increasing evidence that psychological factors, such as busy lifestyle, stress, anxiety and depression, have a negative impact on IVF and pregnancy outcomes.
Research studies have shown that the high levels of stress, anxiety and depression are significantly related to the treatment outcome in IVF and also achieving a natural pregnancy (Expert Review of Obstetrics & Gynaecology.2008- See diagram for how stress affects pregnancy outcomes).
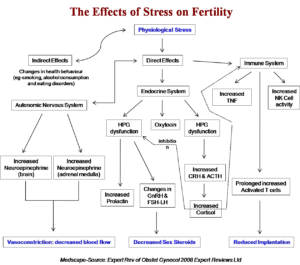
The autonomic nervous system is affected by busyness, stress, anxiety and depression. This also leads to increased neuroepinephrine and increased epinephrine, which then leads to vasoconstriction and decreased blood flow into the uterus. It can also lead to increased stress within the uterus itself.
The immune system is also affected by increased Tumour Necrosis Factor (TNF), which is a cell signalling protein (cytokine) involved in systemic inflammation. The immune system is also affected by increase in Natural Killer Cells and increased activated T cells, which then lead to reduced implantation and a stressed uterine environment.
The indirect effects of stress are that people will drink more alcohol, smoke, exercise less, sleep less, eat more junk foods and generally have a poor diet and lifestyle, all of which have a direct effect on fertility also.
In summary
In summary, lifestyle interventions and taking care of one’s emotional wellbeing can help reduce stress, anxiety and adrenaline. This should be a priority for all couples trying to conceive, or for those having difficulties conceiving. Body-Mind Medicine and Traditional Chinese Medicine have long understood that stress, diet, lifestyle and emotional factors are a huge cause of infertility. Modern medicine and research is now validating this and advocating for proper preconception care. By addressing the known possible emotional and lifestyle factors that affect fertility by utilising preconception care and a multimodality approach (including counselling and psychology), people can greatly improve their fertility, successful pregnancy outcomes, as well as improve their overall health.
Final Word
If you are having trouble conceiving please call our friendly staff and find out how our fertility program may assist you in having a baby. Our fertility program uses a multimodality, ‘no stone left unturned’ approach which looks at both the male and female aspects of fertility, is used alongside medical interventions, and also gives you access to counsellors and psychologists who have a special interest in fertility.
Regards
Andrew Orr
-No Stone Left Unturned
-Master of Reproductive Medicine
-The International Fertility Experts
-The Experts Program
References
- Paulson JF, Bazemore SD. Prenatal and Postpartum Depression in fathers and its association with maternal depression: a meta-analysis. JAMA. 2010;303(19):1961-1969. doi:10.1001/jama.2010.605
- Effects of caffeine, alcohol and smoking on fertility, http://yourfertility.org.au/resource/effects-of-caffeine-alcohol-and-smoking-on-fertility/
- Evans J, Heron J, Francomb H, Oke S, Golding J. Cohort study of depressed mood during pregnancy and after childbirth. BMJ. 2001;323(7307):257-60.
- Akioyamen LE, Minhas H, Holloway AC, Taylor VH, Akioyamen NO, Sherifali D. Effects of depression pharmacotherapy in fertility treatment on conception, birth, and neonatal health: A systematic review. Journal of Psychosomatic Research. 2016;84:69-80.
- Cesta CE, Viktorin A, Olsson H, Johansson V, Sjolander A, Bergh C, et al. Depression, anxiety, and antidepressant treatment in women: association with in vitro fertilization outcome. Fertility and Sterility. 2016;105(6):1594-602 e3.
- Sejbaek CS, Hageman I, Pinborg A, Hougaard CO, Schmidt L. Incidence of depression and influence of depression on the number of treatment cycles and births in a national cohort of 42,880 women treated with ART. Human Reproduction. 2013;28(4):1100-9.
- Ververs T, Kaasenbrood H, Visser G, Schobben F, de Jong-van den Berg L, Egberts T. Prevalence and patterns of antidepressant drug use during pregnancy. Eurpean Journal of Clinical Pharmacology. 2006;62(10):863-70.
- Grigoriadis S, VonderPorten EH, Mamisashvili L, Tomlinson G, Dennis CL, Koren G, et al. The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. Journal of Clinical Psychiatry. 2013;74(4):e321-41.
- Deave T, Heron J, Evans J, Emond A. The impact of maternal depression in pregnancy on early child development. BJOG. 2008;115(8):1043-51.
- Ross LE, Grigoriadis S, Mamisashvili L, VonderPorten EH, Roerecke M, Rehm J, et al. Selected pregnancy and delivery outcomes after exposure to antidepressant medication. A systematic review and meta-analysis. Outcomes after antidepressant use in pregnancy. JAMA Psychiatry. 2013:1-8.
- Rich-Edwards JW, Spiegelman D, Garland M, Hertzmark E, Hunter DJ, Colditz GA, Willett WC, Wand H, Manson JE. 2002. “Physical activity, body mass index, and ovulatory disorder infertility.” Epidemiology 13:184-190.
- Palomba, S, Falbo A, Valli B, et al. 2014. “Physical activity before IVF and ICSI cycles in infertile obese women: an observational cohort study.” Reproductive Biomedicine Online, 29(1): p. 72-9.
- Ferreira RC, Halpern G, Figueira Rde C, Braga DP, et al. 2010. “Physical activity, obesity and eating habits can influence assisted reproduction outcomes.” Womens Health [Lond Engl] 6:517-524.
- Kucuk M, Doymaz F, Urman B. 2010. “Effect of energy expenditure and physical activity on the outcomes of assisted reproduction treatment.” Reproductive Biomedicine Online 20:274-279.
- Morris SN, Missmer SA, Cramer DW, Powers RD, McShane PM, Hornstein MD. 2006. “Effects of lifetime exercise on the outcome of in vitro fertilization.” Obstetrics and Gynecology 108:938-945.
- Green BB, Daling JR, Weiss NS, Liff JM, Koepsell T. 1986. “Exercise as a risk factor for infertility with ovulatory dysfunction.” American Journal of Public Health 76:1432-1436.
- Gudmundsdottir SL, Flanders WD, Augestad LB. 2009. “Physical activity and fertility in women: the North-Trondelag Health Study ” Human Reproduction 24:3196-3204