Tag Archives: Diet & Nutrition
Online Women’s Health Consultations
Do you have Women’s Health issues that you need help with?
Not sure where to go, or who to see?
Sick of healthcare professionals and friends telling you that your symptoms are normal?
Do you just want to see a healthcare practitioner who listens to you and understands your health condition or disease state?
Do you wish you had someone to advocate for you when dealing with other healthcare practitioners?
Wish you had someone to guide you and help you through every step of your healthcare management?
Well, you can have someone not only assist you with your health condition and ongoing healthcare management, but also have someone guide you and hold your hand every step of the way. You will also have access to a trusted network of other healthcare practitioners, if needed.
Why risk trying to do all this on your own, or waste time and money on things that are not helping, or people who are not really listening to you. So many people try to do this on their own, or leave it up to their google search in finding someone. This really is not a great way of finding a good healthcare practitioner.
Exercises For Better Sex
As a practitioner with a special interest in the area of reproductive and sexual health, I thought it’s was time to talk about what you can do to have better sex. While good food, healthy lifestyle, mindfulness and reducing stress can help with improving the sex life and your libido, many exercises can also benefit your sexual health too. These exercises also have other benefits, while making feel good and feel healthier at the same time.
1. Cardio – Getting physical can ramp up the pleasure for you and your partner. Any activity that gets your heart beating faster and you breathing harder, from brisk walking to cycling, can boost blood flow — including to your nether regions. That’s a plus for both genders: stronger erections for men, and greater arousal for women (a whopping 169% more in one University of Texas study).
2. Weight training– Using compound lifts such as dead lifts, squats, bench press etc, all add to strengthening your core, burning fats and strengthening your whole body. They also increase testosterone and other hormones, which help with improving sex drive; increasing orgasm intensity and making you feel good at the same time.
3. Swimming– Harvard researchers found that male and female swimmers in their 60s had sex lives similar to people 20 years younger. Swimming builds endurance, boosts blood flow, improves flexibility and strength, and slashes stress. It also burns some serious calories, a plus for anyone who’s overweight (extra pounds lower libido), especially obese men with erectile dysfunction.
4. Core & Abs Work– A strong, flexible core underpins most everything you do. That includes performing between the sheets. Bonus: You may be one of the lucky people who can have an orgasm while exercising — sometimes called a “coregasm.” It tends to happen during core-strengthening workouts like crunches. Pilates is a great way to work on core and abs.
5. Kegels, Ba Wan Balls and Yoni eggs– Kegels was developed to treat urinary incontinence, these strengthen your pelvic floor muscles, and that means explosive orgasms. Yoni eggs and Ba wen balls have been around for centuries to help with developing muscles in the vagina and pelvic floor and also helping with lubrication, increased circulation and also stimulation of certain hormones such as oxytocin (the love hormone). These exercises and eggs/balls may also help with gynaecological conditions such as Adenomyosis and endometriosis too, alongside medical interventions, by increasing blood flow and assisting with pain. Women may be more familiar with Kegels balls, but probably less familiar with Yoni Eggs and Ba wen balls. Kegels exercises may also help men prevent premature ejaculation. (Always consult with your healthcare practitioner before using kegels balls, yoni eggs and ba wen balls)
6. Plank– This is a perfect way to strengthen the deepest layer of your ab muscles (transversus abdominis), along with your upper arms, thighs, and buttocks. These muscles help stabilize you so you can stay close to your partner when and where it counts most. Do it once a day, and build up to 60 seconds or longer. If it’s too challenging on your toes, try balancing on your knees instead.
7. Cat/Cow Stretch– Think of this yoga pose as another form of foreplay. It limbers your spine, helps get you into an even breathing rhythm, and improves focus — so your mind stays in the moment. Move with a steady flow, so that each rounding up (the cow part) takes a full breath out and each arching downward (the cat part) takes a full breath in.
8. Pelvic Thrusts – Whether your favourite position is missionary or cowgirl, this move is a key part of it. But powerful pushes can be exhausting when you’re out of shape. Work your glutes, calves, and hamstrings to build stamina and flexibility. Pelvic thrusts also sculpt your booty, so you feel good and look good.
9. Better Together– Couples who sweat together stay together; so make an exercise date with your significant other. Studies show that challenging physical activities spark arousal. You’ll be more attracted to your partner post-workout, too. Coordinate your actions (for example, run at the same pace) to strengthen your emotional connection even more.
As I always say to couples, is that having a healthy sex life is so important to a relationship and so vital to connection for the couple. Healthy couples have healthy sexual function and healthy libidos, so healthy diet, mindfulness and a healthy lifestyle is so important to maintaining a healthy sex life. Healthy couples also have healthy babies.
Regards
Andrew Orr
-Leaving No Stone Unturned
-Women’s and Men’s Health Advocate
-Master of Women’s Health
-The Women’s Health Experts
Alcohol Decreases Fertility & Makes Gynaecological Conditions Worse
In today’s modern society, alcohol has become the cornerstone for social engagements, business dinners and after work relaxation. It is important to realise however, that alcohol can directly impact the fertility of both males and females.
In males it can decrease sperm quality, reduce testicular size, decrease libido and cause impotence, all of which can impair fertility.
In females it has a more systemic response, affecting the reproductive hormones, leading to abnormalities in the menstrual cycle and an increased risk of miscarriage.
Effect of Alcohol on Conception for Men
Fecundability refers to the probability of conception during a particular menstrual cycle. It is dependent on the reproductive potential of both partners. Alcohol decreases fecundability by its effect on sperm quality and quantity.
Men who continue to consume alcohol on a regular basis, can decrease their sperm motility, morphology and their DNA in the sperm. All of which are important factors in achieving fertility. While outwardly a man’s sperm may look OK, many forget that inwardly, the sperm DNA could be highly fragmented and unless this is tested every ejaculation, you will have no idea how bad the sperm actually is.
A one off DNA fragmentation analysis does not mean the sperm each time is OK. It only measures the sperm from the ejaculate that was tested and sperm quality can change by as much as 20% each ejaculation.
Testicular size is also affected by alcohol intake; and can also affect sperm production. Alcohol is a depressant of the central nervous system (CNS), and can disrupt the autonomic system of the CNS. These effects are temporary and short lived. Abnormal sperm production is also temporary and also can resume after abstaining from alcohol.
One study, this one looking at couples going through IVF treatment, found that for every additional drink a man consumed per day, the risk of conception not leading to a live birth increased by 2 to 8 times. This was especially true if the drinking occurred within a month of the IVF treatment.
Effect of Alcohol on Conception for Women
In women, alcohol affects fecundability, by disrupting the delicate balance of the menstrual cycle. Clinical research data published in the “British Medical Journal” suggests that women, who drank socially, 1-5 drinks per week, were at a greater risk of decreased fecundability when compared to women who remained abstinent. These findings underscore the importance of remaining abstinent while attempting to conceive.
Alcohol disrupts the hormonal imbalance of the female reproductive system, leading to menstrual irregularities, and even Anovulatory cycles, (menstrual cycles where ovulation fails to occur).
Menstrual pain can directly be linked to the amount of alcohol consumed in the lead up to the menses and consumptions of alcohol, even small amounts, exacerbates most gynaecological conditions. These changes can drastically decrease a woman’s chance of becoming pregnant and thus affect fertility.
Alcohol effects fertility in both partners, and can do so in so many ways. For couples who desire to have a baby, it is best to stay away from drinking completely. Presently there is no safe limit of alcohol intake; even socially acceptable amounts of alcohol can affect fertility potential and outcomes.
Moderate drinking (1-2 drinks in one sitting) is probably okay, especially if you reserve those drinks to a few times a week, instead of daily. However, if you’re going through IVF treatment, or trying to conceive naturally, you might consider cutting out alcohol for the time being.
Trying to conceive is a special time in a couple’s life, it should be filled with love, devotion and safe health practices, which means a healthy diet and lifestyle and having a healthy mind too.
A healthy preconception care program is also a great idea for those trying to increase their fertility and get their reproductive systems working better. Healthy eggs and health sperm make healthy babies. Healthy reproductive systems also mean better menstrual cycles and better testicular health too.
If you would like to book in a consultation with me, or find out more about my fertility program, please call my friendly staff, or using the automated emails system on the website.
You can also make a meet and greet appointment to find out more about the how I can help and assist you and found out about the fertility program too.
Regards
Andrew Orr
-Leaving No Stone Unturned
-Women’s and Men’s Health Advocate
-The International Fertility Experts
Endometriosis Awareness- Ending The Silence
My main aim is to bring awareness about Endometriosis also end the silence for sufferers of this disease that is often overlooked and often ‘missed’ and ‘dismissed’. It is an issue myself as an Endometriosis Expert feels very passionately about.
I help and care for women suffering from this disease every day and I hope that one day, endometriosis can be a word of the past. There is no cure for this disease, but we need to find one.
Through awareness and education, let’s try and get women the early intervention and help they need sooner, rather than later.
What is Endometriosis
Endometriosis, which is an inflammatory gynaecological disease, by which endometrial like tissue grows outside the endometrium. It can spread outside the endometrium into the pelvis, bowel and intestines. It has even been known to get into the brain, joints and around the heart.This disease affects 1 in 10 women, often causing immense pain for them.
According to the Royal College of Obstetricians and Gynaecologist Guidelines for the Management of Endometriosis, it can cause the following symptoms:
Heavy Menstrual Bleeding
Period Pain
Pain with sex
Ovulation Pain
Irritable bowel like symptoms
Bladder issues
Chronic fatigue
Pain with bowel movement
The disease can also cause other symptoms such as :
Bloated belly that looks pregnant around your period (known as endo belly)
Bloated belly that looks pregnant and you are told it is from certain foods, but it isn’t, or may be a combination of food and inflammation from endometriosis (also known as endo belly)
UTI like symptoms that aren’t a UTI
Bleeding from the bowel with your period
Low Iron with no explanation
Being told you have IBS, but you don’t have IBS
Migraines/Headaches that are worse around your period
Irrational mood swings
There are so many other symptoms that could also be pointers to endometriosis.
This disease can also play major havoc with hormones and the libido. Many women with can have pain on intercourse which further lessens the desire around sex.
Women with endometriosis often have painful periods and can’t get out of bed, so if you experience this, there is a good chance that you actually have it.
Women with endometriosis can also have other hormonal disturbances such as mood swings, fatigue, restlessness etc. They can also have other symptoms such as migraines, headaches, dizziness, constipation, pain with bowel movements, joint pains and all manner of symptoms created from the inflammation that endometriosis is caused by and also creates
How Many Women Suffer from Endometriosis?
Endometriosis has now reached an all time high in its ever-growing presence. While the current research says that 1 in 10 women are affected by endometriosis, as an endometriosis expert, I believe, as do many others, that these figures may be grossly under exaggerated.
Research also shows that a significant portion of women affected with endometriosis are asymptomatic (no symptoms) and may only ever get diagnosed if they are having issues with having a baby, or they may never be diagnosed at all. In addition to this, many women diagnosed with Irritable Bowel Syndrome actually have endometriosis and not IBS.
Many women have also been told period pain is normal and hence many never seek help for a condition that can be debilitating on their life and those around them. Women who suffer period pain and other menstrual related symptoms caused by endometriosis are often ‘missed’ and ‘dismissed’ by multiple healthcare professionals and it can take up to 12 years from onset of symptoms to a definitive diagnosis being made.
Women with period pain caused by endometriosis have to live a life of pain, trauma and physical and emotional torment. Many of these women are barely getting through a day, let alone a whole month of exhausting symptoms related to this disease. Some sadly even turn to suicide.
The Western Medicine Approach on the Causation and Treatment of Endometriosis
To date, Western medicine does not know how or even why endometriosis occurs. New research is showing that the disease is a genetic disease that is hereditary.
The only solution that has been offered in the past was to laser it. This usually has a recurrence rate of up to 80%.
The proper way that this disease should be removed is by excising it (cutting it out), which offers better relief with less recurrence.
I do need to stress that when a surgeon is needed, it needs to be done by an advanced trained laparoscopic surgeon, who has had extra specialised training, and is an expert in endometriosis excision and management, and is not just any obstetrician/gynaecologist (OB/GYN). This is where many go wrong and haven’t had the disease dealt with properly.
Despite the increased success in treating endometriosis through a surgical procedure, it still usually reoccurs in a majority of women. There is no cure for endometriosis. To find out more about the facts about endometriosis please click on the link- The Facts About Endometriosis
So why isn’t the medical option alone working?
Primarily it is because they are just treating the symptoms and not the cause. You can take away most physical symptoms very easily, but if the real cause isn’t addressed at the same time, you have no chance of a full recovery. This includes emotional factors.
In addition, many of the hormones that women are put on after surgery, mask the problem and can actually make it worse. By actually stopping the the normal menses, like many of these hormones do, there can be increased risk of further endometriosis growing. Sure, while you have no period, you may have no pain or symptoms, but internally it is still there waiting to flare up again.
Oral contraceptive pills containing estrogen should be avoided as they only add to making the problem worse. Progesterone only options should be looked at rather than a combined pill, if using hormones. These treatments also have limitations that include side effects in some women and contraceptive action for women desiring to conceive.
The Traditional Chinese Medicine Approach on the Causation & Treatment of Endometriosis
Firstly, I can only pass on what the Chinese have known and studied for 10,000 or more years, much longer than western medicine. They had the body and its internal organs mapped out longer before medical science in the west did.
In Chinese Medicine, they believe the liver governs the menstrual cycle, and that it also governs our emotions.They believe that through poor diet, lifestyle, medicines, environment etc, that these can then cause disruption to an organ in the body. Emotions such as anger, frustration, resentment, stress, irritability etc, are believed to cause the liver to be in disharmony.
In Western Medicine terms, we know that poor diet and emotional factors can unlock predisposed hereditary issues, or dispositions through DNA recoding. Yes, diet can affect your DNA coding and so can emotional issues. Similarly we can reverse some disease states, and reprogram DNA coding through a healthy diet and fixing our emotional health.
When the liver is in disharmony, Chinese medicine believes it can cause blockages in our system. Western medicine now also believes that emotions can cause physical symptoms and we often see this is psychiatric, or body-mind medicine. These blockages then cause what we call stagnation.
Chinese medicine believes that when the Qi (energy) becomes stagnant, it causes what they call Liver Qi Stagnation, and this is the cause of many gynaecological conditions such as endometriosis and PMS.
Chinese Medicine believes that when Qi stagnation is left long term, it then affects the blood and turns it stagnant too. Imagine damming a river and the longer the water sits, the more stagnant it becomes because it no longer flows. This is where the term “Blood Stagnation” comes from and what Chinese Medicine believe endometriosis is manifested from.
When we look at endometriosis, it does present as blood clotting and pain. Basically it is like a varicose vein that has all that old, stagnant blood in it. The circulation is no longer moving and the blood now turns dark and causes pain.
Chinese medicine believes that not only is diet and herbal medicine needed to move the stagnant blood and help prevent the disease further expressing itself, but also believes that the emotional component behind it also needs to be addressed.
In Chinese medicine they use lots of warming and blood thinning herbs that are also anti-coagulants, but are also anti-spasmotics. The Chinese medicine also has herbs to help the liver function and also help with emotional wellbeing.
Dr Andrew Orr’s Recommended Approach to Treating Endometriosis
Endometriosis has a highly variable disease state, and thus a multi-modality approach is needed to treat it. Targeting different pathways is likely to be important to move toward precision health (personalised medicine) in endometriosis. People with endometriosis need a team of people looking after them, not just one person and one approach.
For severe cases you will need to see a good advanced laparoscopic surgeon to get as much of the endometriosis excised (cut out-not lasered). Surgery is a much needed option if the pain is severe because it helps removed the deposits (lesions) of the endometriosis that can be seen.
However, it does not deal with the microscopic implants of endometriosis that can’t be seen, and this is why endometriosis is likely to occur again. We do know that despite the best medical interventions that women who have endometriosis can still be in pain and endure the terrible associated symptoms of the disease as well.
Acupuncture and Chinese Medicine may be able to assist with endometriosis and the associated symptoms of this disease . There is now some good anecdotal evidence to suggest that Acupuncture and Chinese herbal medicine may assist with the causes of period pain. This should be done along side medical treatments as well.
To support my view on the treatment of endometriosis, the Royal College of Obstetricians and Gynaecologists guidelines for treating endometriosis now states that Acupuncture and Chinese Herbal Medicine may assist in the management of endometriosis and should be considered.
Following the correct diet and restoring good gut bacteria and gut health (the microbiome) may also help with inflammation and the associated gut related symptoms of endometriosis.
The modern Western diet consists of many foods with high GI levels, causing inflammation to the body and therefore fuelling conditions such as endometriosis. There are all sorts of diets out there attesting to be the cure for endometriosis, but half are them are actually making it worse. A low GI /Low inflammatory based diet may help with assisting the treatment and management of endometriosis and its associated symptoms.
Lastly, see a good counsellor. Different modalities may help both the physical & emotional side of many disease states, but sometimes solution-based talk therapy is needed for the best results.
I provide patients with a list of preferred counsellors and psychologists when I see them for their initial consultation. I always look at the emotional side of everyones health and wellbeing.
A multi modality approach does help, but for anything to work more effectively, you too, have to make a commitment. It is also about finding your team and the team of people right for you too.
Who I am and Why this Means so Much to Me
I am a healthcare practitioner with over 20 years of experience in assisting Women’s Health Medicine and helping women with care and managing endometriosis and its associated symptoms. I know all too well the trials and tribulations women have to go through before someone actually listens and gives these poor women a proper diagnosis.
I also have loved ones with this disease and have also lived with a chronic painful disease too. While I may not fully understand and feel what women with endometriosis actually goes through, I do know what it is like to live daily life with a painful chronic inflammatory disease that can rule your life on every level.
The one thing I do want all women to know is that “Period pain IS NOT normal” and all too often women are told that period pain is normal. Nothing could be further from the truth. We need to educate women and young girls that period pain is not normal.
I have a motto of “Leaving No Stone Left Unturned” and I apply this to every patient I see with period pain, and those potentially suffering from endometriosis.
I would like to see better education and awareness for the general public, but I would also like better education and awareness for healthcare professionals. I would like to see all healthcare professional use my motto and make sure that no woman is ever ‘missed’, or ‘dismissed’ with this horrible disease ever again.
I would like to conclude with one last message. Women need to know that period pain IS NOT normal and that early detection and early intervention and treatment is the key to treating any disease properly. The earlier a woman is investigated and the disease is detected and managed properly, the better her future health and fertility outcomes are.
Please do not think that teenage girls are too young to have endometriosis. Early intervention and early treatment and management of this disease is crucial.
Lets end the silence about this horrible disease. Please support Endometriosis Awareness and support anyone bringing awareness and education about this disease that so many women now have.
If you would like to book in a consultation with me, please call my friendly staff, or using the automated emails system on the website. Let me hold your hand and care for you and assist you in every step of the way to better health and a better way to live daily.
Regards
Andrew Orr
-Women’s and Men’s Health Advocate
“Leaving no Stone Unturned”
“Period Pain IS NOT normal”
Time to Set The Records Straight about Endometriosis, Period Pain & Other Gynaecological Issues.
There are so many misperceptions and wrong information out there about period pain and gynaecological conditions that cause period pain and it really gets annoying hearing people get told the wrong information and false information. It is time we get people the help they need and stop people having gynaecological conditions missed and being dismissed also.
So lets set the records straight
- Period pain is not normal, no matter what you have been told, or who has told you this.
- Period pain is often the sign of gynaecological conditions such as endometriosis, adenomyosis or other gynaecological issue. It could also be a sign of something more sinister.
- Women who have endometriosis and other gynaecological issues, can also be asymptomatic (meaning no symptoms) so because you do not have pain, does not mean that you do not have it.
- With endometriosis, symptoms do not always correlate to the extent of the disease. Some women have only small visual pockets of it and this can cause extreme pain and inflammation, while women whom are riddled with it may have little, or no pain at all. It is not about the amount of the disease when it comes to pain profiles and classifications around pain and disease management. The classification system and grading system is just for a surgeons reference only and to gauge how much was found.
- Scans and blood tests cannot diagnose endometriosis. There are some specialised scans that can diagnose deep infiltrating endometriosis only, but even then, they are not 100% accurate, or a definitive diagnosis. There are very few people trained in this form of ultrasound too. Most women with endometrosis have the superficial disease, which cannot be diagnosed with specialised ultrasound , or normal ultrasound at all. Blood tests will definitely not diagnose endometriosis, or many other gynaecological issues either.
- The definitive diagnosis for endometriosis and other pelvic pathology is a Laparoscopy ( usually combined with hysteroscopy and dye studies) combined with histology (tissue from a biopsy). At the time of laparoscopy the visual disease is usually tidied up and removed at the same time, along with any adhesions and other pelvic pathology found.
- Not all gynaecologists, or surgeons can perform proper surgery needed for the removal of endometriosis, or other gynaecological issues. This requires an advanced laparoscopic surgeon to do this kind of work and not every gynaecologist, or surgeon has these skills.
Many gynaecologists have very limited surgical skills when it comes to major gynaecological issues such as endometriosis. Just because someone has had surgery before, doesn’t mean they have had someone specialised to deal with the disease properly. This is a big mistake many people do not realise.You also always need to ask if the surgeon has advanced laparoscopic training and they excise (cut out) the disease, not burn it. You also need to ask their experience in treating and managing the disease state that you have been diagnosed with, or suspected of having.
Some endometriosis may be so widespread it may need multiple surgeons, such as bowels surgeons, and in some cases it may need a gynaecological oncologist who can excise very fine parameters because of their training of cancer removal. Many women think they have had the disease removed when in fact their surgeon was unable to fully remove all the disease because it was out of their scope of practice.
- Teenagers are not too young to have endometriosis, or other gynaecological conditions. Early intervention and management of the disease is crucial and should not be left until later in life under any circumstances. Please do not let teenagers put up with period pain and have someone tell them it is normal.
- Surgery does not cure endometriosis. But it does help to control the spread of the disease and the inflammation because of the disease.Surgery can offer great relief from pain symptoms though. But the real treatment comes from trying to suppress the regrowth of the disease and microscopic implants (not visible to the eye via surgery) post surgery and this is what I do in my treatments.
- Pregnancy does not cure endometriosis, or period pain. In many cases, it can make it slightly better for a while, but most of this is due to women not having their period for an extended amount of time. It does not cure endometriosis and this is a widely spread myth that needs to be corrected
- Endometriosis is not an auto-immune disease. Lately there has been talk that endometriosis is an autoimmune disease because of its inflammation links. Yes, it is an inflammatory disease and reducing inflammation in the body will help it, but it is not an auto-immune disease and does not fit the classifications of an auto-immune disease either.
- Gynaecological conditions should be seen to by a specialist in that field and not just by a GP. While GP’s are a much needed part of healthcare, but they are just a general practitioner, they are not a specialist and a referral to a properly trained specialist should be obtained for any suspect gynaecological condition, or matters pertaining to period pain, or pelvic pain. This saves conditions being missed, or overlooked, or misdiagnosed
- Hysterectomy does not cure endometriosis. Most of the time endometriosis is outside the uterus and can be anywhere in the pelvic cavity. It can be on the bladder, the bowel, the fallopian tubes and it can even spread to anywhere in the body. Endometriosis has been found in the joints, around the heart, the brain and even in the eyes. Taking the uterus out is not going to cure endometriosis.
Lastly, Dr Google and many of the forums people use are not usually reliable sources of information, or a diagnosis for period pain, gynaecological conditions such as endometriosis, or any other gynaecological conditions.
Only a properly trained Reproductive Medicine Specialist, Gynaecologist, Fertility Specialist, or Women’s Health Medicine Specialist can give you proper advice and education about endometriosis and matters that pertain to women’s health.
Your next door neighbour, your friend, your Facebook buddies are not reliable sources of information, unless they are fully qualified healthcare professional. There are some good sites out there, but even so, you still need to get advice of a proper healthcare professional and not just some person on a forum, or internet site.
I hope this helps people understand the importance of the right information and education and seeing the right people and getting investigated and managed properly. I see so many people have things missed, dismissed and overlooked and I just want to help people get the right advice and right treatments and be given the right information to save people on the heartache that many I have seen have had to endure.
My motto will always be that “Period Pain is Not Normal” and my other motto is “Leaving No Stone Left Unturned” when it come to healthcare and helping people. If someone tells you period pain is normal, or you have to put up with it, or suck it up, you are seeing the wrong person, so please then go and see someone else.
If you would like to book in a consultation with me, please call my friendly staff, or using the automated emails system on the website. Let me hold your hand and care for you and assist you in every step of the way to better health and a better way to live daily.
Take care
Regards
Andrew Orr
-No Stone Left Unturned
-Women’s and Men’s Health Advocate
-Period Pain is not normal
Vitamin D deficiency increases risk of chronic headache
New studies have shown that Vitamin D deficiency can increase the risk of chronic headache, according to a new study from the University of Eastern Finland. These new findings were published in he journal – Scientific Reports.
The researchers from the Kuopio Ischaemic Heart Disease Risk Factor Study, KIHD, analysed the serum vitamin D levels and occurrence of headache in approximately 2,600 men aged between 42 and 60 years. The research showed that in 68% of these men, the serum vitamin D level was below 50 nmol/l, which is generally considered the threshold for vitamin D deficiency. Those with low levels of Vitamin D were more prone to Chronic headache occurring at least on a weekly basis.
In Australia over 97% of the population are known to be Vitamin D deficient. This is because we are now staying indoors longer and sunscreens are also blocking some of the absorption on this necessary vitamin. Plus, you need to be outside in the sun at certain times of the day, for certain periods, without sunscreen on for proper absorption to occur. Our diet is another source of vitamin D and we are also lacking there.
Vitamin D deficiency is also linked to other chronic disease states and is a big part of people developing osteoporosis. Vitamin D is very much needed for healthy bones and also a healthy immune system
At my clinic I have helped and assisted people with all sorts of Vitamin, Mineral and Nutrient deficiencies. I also carry a high potency practitioner only Vitamin D supplement that may assist in getting your Vitamin D levels back to where they should be.
If you would like to book in a consultation with me, please call my friendly staff, or using the automated emails system on the website. Let me hold your hand and care for you and assist you in every step of the way to better health and a better way to live daily.
When was the last time you got your Vitamin D levels checked?
Regards
Andrew Orr
-Leaving No Stone Left Unturned
-Women’s and Men’s Health Advocate
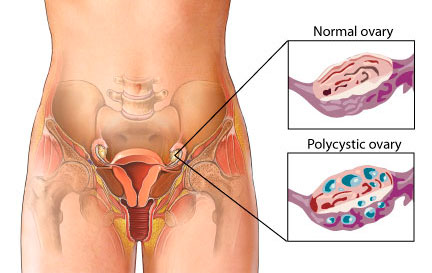
Women with PCOS often have to wait 2 years and often see multiple healthcare professionals before diagnosis is made
Polycystic ovary syndrome (PCOS) is the most common endocrine/gynaecological/reproductive disorder — and most common cause of infertility — affecting 9 to 18 percent of women around the world.
Despite the prevalence of this chronic condition, one-third of women diagnosed with PCOS saw at least three health professionals over the course of two years before receiving a diagnosis, according to a study from the Perelman School of Medicine at the University of Pennsylvania.
The study, published in the Journal of Clinical Endocrinology & Metabolism, is the largest to date examining time to diagnosis, and reveals what the authors say are “major gaps” in education and support for women with the condition.
As a healthcare practitioner with a special interest in this area, I see these same issues with so many women waiting years to get a proper diagnosis and they have seen multiple healthcare professionals in both the medical and complementary medicine profession.
The signs and symptoms of PCOS are very clear and easily diagnosed, but many healthcare professionals end up focussing on one symptom, while overlooking the bigger picture and then these poor women get their condition missed.
Many practitioners and public alike, do not understand the difference between PCO (Polycystic Ovaries) and PCOS (Polycystic Ovarian Syndrome) either and this creates a big issue as well. These days the two condition are actually put under the heading of the one condition, when this is not entirely true. For more information about PCO and PCOS, please click of this link (click here)
PCOS primarily affects women of reproductive age — most often between the ages of 18 to 35. The most common signs of PCOS are:
- Absent, Irregular and Inconsistent menstrual periods,
- Acne
- Excess hair growth (some women can have hair loss too)
- Central obesity
If a women presents with Acne, irregular periods, absent periods etc, there is a good chance that she may have PCOS. The problem for these women, as explained before is that healthcare providers and placing too much emphasis on only one of these symptoms, which is usually the Acne, or just that the cycle is irregular. Then women are then put on the Pill and these symptoms are masked for years, until they try and have a child and have difficulty doing so.
Women with PCOS also have an increased risk of type 2 diabetes, gestational diabetes, metabolic syndrome and anxiety and depression, and studies have shown that the longer it takes for the condition to be diagnosed, the greater the patient dissatisfaction.
These new results are concerning for those of us who do know how to deal with PCOS and other gynaecological conditions properly. These women should not be having this conditions missed. The other issue is that not only do women often wait several months or even years before care providers are able to diagnose the condition, but even after diagnosis, patients are often unsatisfied with the information and support they receive. It is such a vicious cycle.
But let’s not forget out Endo Sister’s who have endured the long road to diagnosis and management for their disease. It can often take up to 12 years for their diagnosis and again many of them have their condition missed and are dismissed. It is again such a vicious cycle of mismanagement and focus one symptoms before someone finally properly diagnoses their disease. Then many of these also complain of the management and treatment after diagnosis. We also know that many with endometriosis, also have PCOS. These two disease states can go hand in hand and both can equally be missed and dismissed.
Based on the study findings, the authors are calling for the development of international evidence-based guidelines, co-designed consumer and health professional resources and international dissemination to improve diagnosis experience, education, management and health outcomes.
Too right they should be calling for better diagnosis and better education and training for these healthcare professionals. If you don’t know how to do your job properly, or it is out of your scope of practice, get out of the way and refer these women onto people who are trained to diagnose and manage these conditions properly.
Lets, help put and end to PCOS and also put an end to Endometriosis as well. Let’s break the silence and help women get the diagnosis and care they need. Early intervention and treatment is crucial for any disease state and let’s help women get this care sooner.
Take care
Regards
Andrew Orr
-Women’s and Men’s Health Advocate
-“Period Pain IS NOT normal”
-“Leaving no Stone Left Unturned”

Journal Reference:
Melanie Gibson-Helm, Helena Teede, Andrea Dunaif, Anuja Dokras. Delayed diagnosis and a lack of information associated with dissatisfaction in women with polycystic ovary syndrome. The Journal of Clinical Endocrinology & Metabolism, 2016; jc.2016-2963 DOI: 10.1210/jc.2016-296
How the Christmas, New Year & Easter Festive Seasons Can Affect a Woman’s Menstrual Cycle
We have not long gotten over the Christmas and New Year period and we are about to embark on the fast train into Easter holiday and festive season.
While many are getting ready for the sugar fest ahead, with Easter eggs and hot cross buns galore, we need to take the time to understand how this may affect our bodies afterwards, especially for women and their menstrual cycles.
Worse still it could even affect pre-existing gynaecological conditions that women live with on a day to day basis, some of which impact women’s day life terribly.
Christmas and Easter times always pose great problems for women and their menstrual cycle, and year after year many women never make the correlation why.
Year after year I see women coming back to see me, after Christmas and Easter, scratching their heads as to why all of a sudden their menstrual cycle has gone haywire and they are getting the worst PMS symptoms they’ve had since they can remember.
So why do so many women have problems with their menstrual cycle after Christmas and Easter?
The answer is blatantly obvious. Stress, Poor diet and Lifestyle factors!
The lead up to Christmas and Easter, is always a busy time and no matter how much people try to deny it, it is very stressful. People are rushing madly to meet deadlines before everyone goes on holidays and then the mad Christmas and Easter shopping rush that follows.
Then there is the stress of what to buy everyone, followed by the mad catering panic. People literally go mad and one would think the end of the world is imminent, with supermarkets being emptied by the marketing hype of these two festive seasons.
Then the big day arrives. Everyone forgets the basic principles of a healthy diet and engorge themselves on any food they can lay their hands on. Basically it is a licence to eat as much bad food as we can put in our mouths, and then use the basic excuse of “Its Christmas” or “It’s Easter” and “It is only just one day and it won’t really matter and I had to do it”.
Then one day leads into two, and then this leads into a week and then before we know it, it has been more than just one day of bad eating, or drinking alcohol. The sad fact of that statement is that some people eat and drink alcohol like it’s Christmas and Easter every day.
With Christmas we can have many portions of baked dinner, crackling, seafood, Christmas pudding, chocolate and any other sugar substance that can be consumed it all had to be washed down with a nice alcoholic beverage, or two. Many bottles of bubbly, or choice of poison later, and we now have a stomach full of sugar, fat, cholesterol and alcohol all churning quite nicely. Diabetes and heart disease here we come.
Then approximately 1 week later it is New Years Eve and the license, to drink like fish and eat like a ravenous bear, is pulled from the pocket and waived around once more. “But it’s Ok”, we say.
The New Year’s resolution will be to not do it again, until next year when all resolutions are forgotten. Meanwhile the system had short circuited, the gut has gone into melt down, the cholesterol levels are rising, the sugar levels have reached diabetes status and the brain cells have been reduced yet again.
Several months later when the system has started to recover, Easter arrives and the sugar binge begins; with Easter eggs and all manner of chocolate, sugar laden delight. Let’s not forget the alcohol added to the mix, that we used to self medicate from the stress of the lead up to the Easter break. The body short circuits itself again and will take until Christmas to recover and then it starts all over again.
Now, I wonder why the menstrual cycle would be affected?
Hmmm, I wonder?
There are only a few things that will affect a menstrual cycle and cause PMS, irregularities and pain. The trouble is many of them can be unknowingly self- inflicted. Yes, many monthly menstrual related problems can be unknowingly self- inflicted.
Let’s not forget that many people do have gynaecological issues that they suffer on a daily basis though. But even still, this high amount of burden on the system will exacerbate these pre-existing conditions and make them worse, due to the resulting high levels of inflammation.
What I am trying to do is just make people aware of how conditions can be worsened and how these high levels of inflammation, from high levels of sugars etc, can cause havoc with a woman’s cycle. This is not about blame. It is about education and prevention. I am here to help, not hinder. Please remember this.
As I said there are only a few things that affect, or exacerbate, a woman’s menstrual cycle and I’m going to list them below. So that way if you are wondering why you can’t get enough Naprogesic into your body, when you get your cycle, please remember the list below.
Please also read my article on “What a proper Menstrual Cycle Should Be Like”. If it isn’t like the one I describe you better book in to see me soon.
What Affects a Menstrual Cycle
- Poor diet – Foods such as high sugars and junk foods all cause inflammation in the body and lead to hormonal irregularities and pain with the menses
- Alcohol – Most alcohols contain high sugars and they also cause inflammation in the body. It also interferes with your hormones and affects the liver too. In Chinese medicine the Liver governs the menstrual cycle. Excess alcohol leads to SOL ( Shit on Liver)
- Poor Sleep– Sleep deprivation leads to reduction in hormones such as serotonin and then effect the moods etc. Lack of sleep also stops the body from repairing and can lead to other health issues
- Trauma – Things such as surgery, a virus, cold/flu etc, or where the body has to repair, can lead to menstrual irregularities. The body shuts down the menses so that it can repair itself first
- Weight gain or weight loss– It is a well known fact that many athletes do not get a menstrual cycle because of lack of body fat. The same goes for people who are overweight too. Too much, or too little, body fat interferes with your fertility. All your hormones are made from fats and protein.
- Emotional Issues– Bottled up emotions such as anger & frustration cause blockages in the system & then cause pain. Emotional issues, such as anxiety also cause problems with hormones and lead to further pain and inflammation. Emotions can be a major issue in any health condition, or can affect hormones.
What a proper menstrual cycle should be like
A proper menstrual cycle should be 26 –32 days in it’s length. It should be 4 days flow, 5 at the most. Any shorter than 4 days is too short and any longer than 5 days is too long. This isn’t good.
You shouldn’t get any pain at all, you shouldn’t get clotting, spotting, breast tenderness, bloating, fluid retention or changes to the moods such as teariness or irritability. These are all signs of irregularities that may need to be addressed.
Some of the things that exacerbate menstrual issues are listed above.
Lastly, please know that Period Pain IS NOT Normal and neither are some of the other irregularities women have. If you are suffering pain, or irregular cycles, or any other issue that doesn’t seem right to you, you need to get it checked out.
If you would like to book in a consultation with me, please call my friendly staff, or using the automated emails system on the website.
Regards
Andrew Orr
-Master of Women’s Health Medicine
-“Leaving No Stone Left Unturned”
-“Period Pain IS NOT Normal”
-The Women’s Health Experts
-The Experts Program
What Affects a Menstrual Cycle – Part 1 (Non Gynaecological Factors)
After my post on “What a Proper Menstrual Cycle Should Be Like”, I always have lots of people asking what the cause of their menstrual irregularities are.
Most of the causes can be broken into two causes being:
Non Gynaecological Factors– Meaning things you do, or may have done to exacerbate current conditions, or throw your cycles out of balance
Gynaecological Factors– Disease states such as Endometriosis, PCOS, Fibroids, Polyps, Adenomyosis, Cancers and other causes.
I’ll talk about the factors (Non-Gynaecological Factors) in people’s control so that they may be able to identify some of those things they may be doing on a daily basis to exacerbate current underlying issues, or just interfere with their hormones and lead to problems with their menstrual cycle.
These ones you can work on and be aware of in case your cycle isn’t regular, or your pain is worse in a month. This way you can look back and go “Oh….. Now I know why my cycles wasn’t so good this month”
I’ll talk about the Gynaecological Causes of irregular, or painful cycles in my next post. For now here are the Non-Gynaecological causes.
What Affects a Menstrual Cycle- Non-Gynaecological Factors.
- Poor diet – Foods such as high sugars and junk foods all cause inflammation in the body and lead to hormonal irregularities and can exacerbate, or cause pain with the menses
- Alcohol – Most alcohols contain high sugars and they also cause inflammation in the body. It also interferes with your hormones and affects the liver too. In Traditional Chinese medicine, it is believed the Liver governs the menstrual cycle and the Live also controls the emotions. Excess alcohol leads to SOL ( Shit on Liver) and thus the moods and cycle get affected.
- Poor Sleep– Sleep deprivation leads to reduction in hormones such as melatonin, which is a precursor to serotonin and then effect the moods etc. Lack of sleep also interferes with the other hormones in our body too. Lack of sleep also stops the body from repairing and can lead to other health issues. We know that shift works do have a lot more disturbances with their cycles and also have lower fertility rates.
- Trauma – Things such as surgery, a virus, cold/flu etc, or where the body has to repair, can lead to menstrual irregularities. The body shuts down the menses so that it can repair itself first. Emotional trauma can also cause the menses to shut down, or become irregular too.
- Weight gain, or weight loss– It is a well known fact that many athletes do not get a menstrual cycle because of lack of body fat. The same goes for people who are over-weight too. Eating disorders can also cause irregularities and infertility. Too much or too little body fat interferes with your fertility. All your hormones are made from fats and protein.
- Emotional Issues– Bottled up emotions such as anger & frustration cause blockages in the system & then cause pain. Emotional issues also cause problems with hormones. Emotions and stress are a major cause of menstrual irregularities. Bottled up emotions can cause SOL too ☺
- Drugs/Hormones– Both pharmaceutical and recreational drugs can also cause menstrual irregularities and can stop the menses completely. Recreational drugs can also lead to permanent infertility.
- Travel– Travelling over time lines and even just interstate can cause issues with your cycle too. The body has to cope with adjusting to different times zones, different foods and water etc and the pressures from flying can also throw the cycle out.
Hope this help explain a little bit more about how our diets and lifestyle can affect your cycles each month too.
If you would like to book in a consultation with me, please call my friendly staff, or using the automated emails system on the website.
There are options for online consultation for those that are interstate, not local, or those that live overseas. My friendly staff will be able to sort this out for you.
Next I will talk about the gynaecological conditions which can causes issues with your cycle. Stay tuned 🙂
Take care
Regards
Andrew Orr
-“Leaving No Stone Unturned”
-Women’s and Men’s Health Advocate
-The Endometriosis and PCOS Experts