Cervical cancer awareness is something all women need to know about and why proper screening for women is so important. It is so important that we bring awareness to cervical cancer, just as we do to many other cancers such as breast cancer and ovarian cancer.
Cervical cancer remains a significant cause of death, from cancer in women worldwide. In clinic I see so many women with the early, intermediate and sometimes advanced stages of cervical cancer. It isn’t good and many women with early detection on cancer cells aren’t being proactive in follow up consults, or have little idea just how significant these results are to their future health and possible length of their life.
Our increasing understanding of the relationship between HPV infection, pre-invasive and invasive disease of the cervix, the introduction of population screening programs using Pap smear testing, the availability of HPV vaccines, and the introduction of testing for high-risk HPV DNA types have changed the burden of disease in developed countries but even so, cervical cancer remains a significant problem in developing countries.
The Statistics of Cervical Cancer
World wide, cervical cancer is the fourth most common cancer in women, and the 7th most common overall.
In 2012, there were approximately 528 000 new cases of cervical cancer, and there were 266 000 deaths as a result of cervical cancer. In 2015, there were 857 new cases of cervical cancer diagnosed in Australia. In 2019, it is estimated that 951 new cases of cervical cancer will be diagnosed in Australia. In 2019, it is estimated that the risk of a female being diagnosed with cervical cancer by her 85th birthday will be 1 in 494.
The majority of cases (approximately 85%) and deaths (87%) occur in less developed regions.
In Australia a report by the AIHW “Gynecological Cancers in Australia: an overview” showed the following statistics regarding cervical cancer.
-there were 951 cases of cervical cancer, accounting for 1.4% of all gynaecological cancers
– cervical cancer was the 14th most commonly diagnosed cancer in females
– the estimated number of deaths from cervical cancer was 256
– approximately 70% of cervical cancers were diagnosed in women under the age of 60 years
– the risk of being diagnosed with cervical cancer by the age of 85 years was 1 in 494.
HPV and cervical cancer
HPV (Human Papilloma Virus) is a major cause of cervical cancer and why we need to get the safe sex message out there. In a study of almost of 1000 cases of cervical cancer worldwide, the prevalence of HPV infection was 99.7%.
Screening and regular checkup are also needed in the overall prevention and early intervention of this disease. Large population based studies have shown that screening via gynaecological examinations and Cytologic (Pap smear),may decrease cancer incidence and mortality by more than 80%.
The current screening recommendations are:
Routine screening with Pap smears use to be carried out every two years for women who have no symptoms or history suggestive of cervical pathology. Since 2017, the pap test has been done away with and that has now changed to the new cervical screening test.
All women who have ever been sexually active should start having Pap smears between the ages of 18 and 20 years, or one or two years after first having sexual intercourse, whichever is later. In some cases, it may be appropriate to start screening before 18 years of age.
Pap smears may cease at the age of 70 years for women who have had two normal Pap smears within the last five years. Women over 70 years who have never had a Pap smear, or who request a Pap smear, should be screened.
This policy applies to women with no symptoms and normal Pap smear results who should be screened. To find out more about the cervical screening test, you should talk you your healthcare practitioner, or specialist. You can also find out more information about cervical cancer screening at Cancer Australia
National screening and education about regular screening, has had a significant impact on the reduction of cervical cancer and deaths caused by this disease
HPV Vaccination
Please note that HPV vaccinated women would still require cervical screening as the HPV vaccine does not protect against all the types of HPV that cause cervical cancer. Until any changes are implemented women should continue to have two yearly Pap tests.
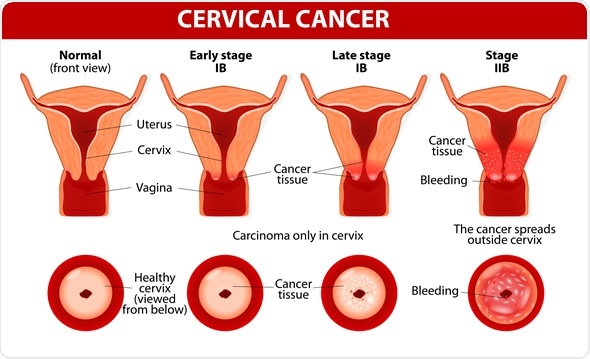
Symptoms of Cervical Cancer
Abnormal vaginal bleeding is the most common symptom of invasive cancer of the cervix. This may include bleeding after sex, bleeding in-between periods, or post-menopausal bleeding.
Cervical cancer is often asymptomatic until quite advanced in women who are not sexually active.
Other symptoms may include:
- Pelvic pain
- Bowel or bladder symptoms due to pelvic pressure
- Symptoms from a fistula (leaking urine or faeces vaginally)
Cervical cancer is preventable
Cervical cancer remains an important preventable cause of cancer in women both in Australia and worldwide. Even with the advent of vaccines, it is very important to remember that participation in regular screening is still necessary and a key part of reducing the incidence and deaths from cervical cancer.
Avoiding risk factors and increasing protective factors will help prevent many forms of cancer
The following risk factors increase the risk of cervical cancer:
1. HPV infection
2. Smoking (even social smoking, or 1-2 per day)
3. DES (diethylstilbestrol) Exposure – A man made estrogen
4. Poor diet
5. Being Overweight
6. Lack of exercise
7. High number of full-term pregnancies
8. Long term use of oral contraceptives
The following protective factors decrease the risk of cervical cancer:
1. Preventing HPV infection
2. Cervical Cancer Screening (pap smears & new HPV screen)
3. Diet (decreasing highly refined foods)
4. Exercise
5. Weight Loss
6. Quitting smoking
Avoiding risk factors and increasing protective factors does help prevent cancers and we all need to look at avoiding the risk factors and increasing more of the protective factors. If you are worried about your risks, you should talk to your healthcare professional about how you might lower your risk of cervical cancer.
Final Word
In practice I see so many women presenting with various stages of this disease and end up not being pro-active around the treatment of the disease. So many take this disease and precancerous cells too lightly. It can kill if not treated properly and therefore it is important to follow up with proper screening, treatments and interventions of cervical cancer.
Let’s bring more awareness to cervical cancer and let’s bring more awareness to prevention and hopefully a cure.
Regards
Andrew Orr
-No Stone Left Unturned
-Master of Women’s Health Medicine
-The Women’s Health Experts