There are so many misperceptions and wrong information out there about period pain and gynaecological conditions that cause period pain and it really gets annoying hearing people get told the wrong information and false information. It is time we get people the help they need and stop people having gynaecological conditions missed and being dismissed also.
So lets set the records straight
- Period pain is not normal, no matter what you have been told, or who has told you this.
- Period pain is often the sign of gynaecological conditions such as endometriosis, adenomyosis or other gynaecological issue. It could also be a sign of something more sinister.
- Women who have endometriosis and other gynaecological issues, can also be asymptomatic (meaning no symptoms) so because you do not have pain, does not mean that you do not have it.
- With endometriosis, symptoms do not always correlate to the extent of the disease. Some women have only small visual pockets of it and this can cause extreme pain and inflammation, while women whom are riddled with it may have little, or no pain at all. It is not about the amount of the disease when it comes to pain profiles and classifications around pain and disease management. The classification system and grading system is just for a surgeons reference only and to gauge how much was found.
- Scans and blood tests cannot diagnose endometriosis. There are some specialised scans that can diagnose deep infiltrating endometriosis only, but even then, they are not 100% accurate, or a definitive diagnosis. There are very few people trained in this form of ultrasound too. Most women with endometrosis have the superficial disease, which cannot be diagnosed with specialised ultrasound , or normal ultrasound at all. Blood tests will definitely not diagnose endometriosis, or many other gynaecological issues either.
- The definitive diagnosis for endometriosis and other pelvic pathology is a Laparoscopy ( usually combined with hysteroscopy and dye studies) combined with histology (tissue from a biopsy). At the time of laparoscopy the visual disease is usually tidied up and removed at the same time, along with any adhesions and other pelvic pathology found.
- Not all gynaecologists, or surgeons can perform proper surgery needed for the removal of endometriosis, or other gynaecological issues. This requires an advanced laparoscopic surgeon to do this kind of work and not every gynaecologist, or surgeon has these skills.
Many gynaecologists have very limited surgical skills when it comes to major gynaecological issues such as endometriosis. Just because someone has had surgery before, doesn’t mean they have had someone specialised to deal with the disease properly. This is a big mistake many people do not realise.You also always need to ask if the surgeon has advanced laparoscopic training and they excise (cut out) the disease, not burn it. You also need to ask their experience in treating and managing the disease state that you have been diagnosed with, or suspected of having.
Some endometriosis may be so widespread it may need multiple surgeons, such as bowels surgeons, and in some cases it may need a gynaecological oncologist who can excise very fine parameters because of their training of cancer removal. Many women think they have had the disease removed when in fact their surgeon was unable to fully remove all the disease because it was out of their scope of practice.
- Teenagers are not too young to have endometriosis, or other gynaecological conditions. Early intervention and management of the disease is crucial and should not be left until later in life under any circumstances. Please do not let teenagers put up with period pain and have someone tell them it is normal.
- Surgery does not cure endometriosis. But it does help to control the spread of the disease and the inflammation because of the disease.Surgery can offer great relief from pain symptoms though. But the real treatment comes from trying to suppress the regrowth of the disease and microscopic implants (not visible to the eye via surgery) post surgery and this is what I do in my treatments.
- Pregnancy does not cure endometriosis, or period pain. In many cases, it can make it slightly better for a while, but most of this is due to women not having their period for an extended amount of time. It does not cure endometriosis and this is a widely spread myth that needs to be corrected
- Endometriosis is not an auto-immune disease. Lately there has been talk that endometriosis is an autoimmune disease because of its inflammation links. Yes, it is an inflammatory disease and reducing inflammation in the body will help it, but it is not an auto-immune disease and does not fit the classifications of an auto-immune disease either.
- Gynaecological conditions should be seen to by a specialist in that field and not just by a GP. While GP’s are a much needed part of healthcare, but they are just a general practitioner, they are not a specialist and a referral to a properly trained specialist should be obtained for any suspect gynaecological condition, or matters pertaining to period pain, or pelvic pain. This saves conditions being missed, or overlooked, or misdiagnosed
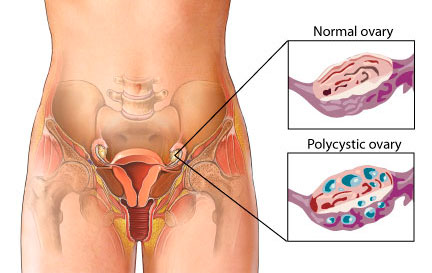
- Hysterectomy does not cure endometriosis. Most of the time endometriosis is outside the uterus and can be anywhere in the pelvic cavity. It can be on the bladder, the bowel, the fallopian tubes and it can even spread to anywhere in the body. Endometriosis has been found in the joints, around the heart, the brain and even in the eyes. Taking the uterus out is not going to cure endometriosis.
Lastly, Dr Google and many of the forums people use are not usually reliable sources of information, or a diagnosis for period pain, gynaecological conditions such as endometriosis, or any other gynaecological conditions.
Only a properly trained Reproductive Medicine Specialist, Gynaecologist, Fertility Specialist, or Women’s Health Medicine Specialist can give you proper advice and education about endometriosis and matters that pertain to women’s health.
Your next door neighbour, your friend, your Facebook buddies are not reliable sources of information, unless they are fully qualified healthcare professional. There are some good sites out there, but even so, you still need to get advice of a proper healthcare professional and not just some person on a forum, or internet site.
I hope this helps people understand the importance of the right information and education and seeing the right people and getting investigated and managed properly. I see so many people have things missed, dismissed and overlooked and I just want to help people get the right advice and right treatments and be given the right information to save people on the heartache that many I have seen have had to endure.
My motto will always be that “Period Pain is Not Normal” and my other motto is “Leaving No Stone Left Unturned” when it come to healthcare and helping people. If someone tells you period pain is normal, or you have to put up with it, or suck it up, you are seeing the wrong person, so please then go and see someone else.
If you would like to book in a consultation with me, please call my friendly staff, or using the automated emails system on the website. Let me hold your hand and care for you and assist you in every step of the way to better health and a better way to live daily.
Take care
Regards
Andrew Orr
-No Stone Left Unturned
-Women’s and Men’s Health Advocate
-Period Pain is not normal