Recently I did a post on over the counter pain medicines and how that as of February 2018, that some of these codeine based pain medicines, will now no longer be available over the counter in Australia. I know that in other parts of the world, these medications are not available over the counter anyway and in some countries even paracetamol is not available as readily as it is here in Australia.
The post surely did get people talking and it surely highlighted some very important points. It also highlighted how many people are in pain daily and something that I have known for a long time. I actually know that pain and people with pain conditions, aren’t managed very well. It also highlighted that many people are self managing pain conditions and that many do not realise that they in fact dependent on medications, alcohol and other drugs. Many also do not realise that the pain and symptoms they are experiencing daily, may in fact be withdrawal and dependence symptoms from their medications and substances they are using, including alcohol, and may have nothing to do with their condition at all. It is a very complex issue and there needs to be more education around this very sensitive issue.
Now, before we get started and before anyone tries to bring the personal/emotional side of things into this, I need to be very clear on this and set some boundaries up front. I need everyone to listen to this, so it is clear and that what I am about to say is coming from personal experience, clinical experience and someone who cares and is just trying to help with the right advice and right education around this issues.
So before we start I need to get a few things straight
- I have lived with a painful condition and have used pain medication and been dependent on pain medications. I have also withdrawn off pain medications
- I have loved ones who have pain conditions, who suffer daily and have also used pain medications to get through their day. Also know many of these have learned to manage and overcome their disease and pain too.
- People in pain, need help to get out of pain and pain medications are one way of doing this
- Many people who are in pain are actually dependent on pain medications and are completely unaware that they are dependent
- It is completely OK to take pain medication when someone is in pain. It just needs to be monitored a little better than it has been in the past.
- Please take the personal out of this and just sit back and listen
- I am not here to judge, or attack anyone
- This post is purely from heart, from caring and also about helping people with education so that they can get help if they need to
- The first part of any change and getting help is admitting you have an issue, or a problem, in the first place.
- The is no guilt, shame, or anything wrong with admitting you have a problem, or a dependency
- For the sake of this post I am going to used the word “Dependency”, rather than the words “Abuse” or “Addict”
- Perception is reality and sometimes ones perception is not reality, or based on all the facts
- Not all pain is from the withdrawal of medications either, but some of it could be.
- We are here to support people and care for people, not attack them. Anyone found attacking another on any posts surrounding this subject, will be deleted.
- Lastly, to get help, you need to see a qualified healthcare practitioner and you should only ever rely on information from a qualified health expert, not from your friends, your support groups, or anyone without a proper qualification in things to do with medical, medicines, or health conditions.
Right, now we have set the boundaries and we are clear, we can move forward and I can start explaining about pain, pain medications, pain pathways and also withdrawal symptoms
Before I start, I need everyone to open, his or her, minds a bit and think of how you feel when you have had some alcohol. Let’s not forget that alcohol is a drug and it can make you feel good initially and then not so good if you have a few glasses, or more. You can also become dependent on it too, and yes, it can be abused.
So, say you have a few glasses of alcohol, how do you feel while you are consuming it and shortly after?
This is for the average person, but most people would feel a little warm and tingling and feel quite good wouldn’t they?
But, even with a few glasses, would you necessarily wake up OK the next morning?
Some people might wake up semi OK, some might feel a little less than OK?
For some, a few are nothing because they are used to having way more. Some of these people may in fact be dependent and actually have an alcohol dependency.
So, say you have more than a few glasses of alcohol, how might you feel the next morning?
More than likely you may feel a little dusty, or for some, you may in fact have what we all know to be a hangover… is that correct?
You might feel really tired, irritable, nauseas, sore, have a headache, or a really bad head that feels like it might explode, and all the senses are just a little on hyper-drive and you would feel a little off??
Now that we are clear that alcohol can give you a hangover and make you a bit sick and that alcohol is in fact a drug, let me ask you this?
If alcohol is a drug and it can give you a hangover, even after one night of taking it, and taking just a few glasses of it, then why would not a medication, that can produce all the initial effects of alcohol, then not cause you a “Hangover Effect” the next day as well????
Just have a think about that for one second and let it really sink in.
Hmmmm, what are you thinking now?
Well, I am sure this is where we get some people going “But, but, but!”
Well there are no “But’s”. This is the hard but honest truth. Any drug, being prescription, over the counter, off the street and illegal, can cause you a withdrawal and hangover effect. Also, the longer you take those drugs, the more you take them etc, the more you need to take and the more dependent you become on them. This doesn’t mean I don’t get why people take these medications. I do get it and I get all the reasons behind it too. This is just to explain everything logically and properly to people so that they also get that they may not be managed properly and that they may also be dependent on medications, which are actually in the long term, making all their symptoms worse, or actually causing the ones they have now.
Just so people don’t forget, please go back to points 1 and point 2 in the ground rules I set before. I have lived with pain and I have loved ones who are in pain and yes, I have taken pain medications and so have my loved ones.
Ok, so we are now all on the same page and are clear here, yes, many of the medications that people are taking daily, or periodically, or once off, or chugging down by the packet load, or are actually causing them rebound symptoms and withdrawal symptoms, when those drugs wear off.
We also need to recognise that some people are only taking medications every so often, when they need them too and this is more for people who are medication daily, or frequently. But even still, people do need to be away of rebound symptoms from taking medications, even periodically.
When we talk about “withdrawal” and “rebound symptoms”, let’s all go back to the alcohol story. We know that the hangover symptoms occur because of a rebound and withdrawal affect from the alcohol messing with the symptom, causing dehydration, causing inflammation and then causing all manner of symptoms from nausea, headaches, tiredness and even muscle and joint pain. The same goes for when you take any pain medications, especially those that are opiates, or contain codeine, or convert to morphine in the body.
Are we all getting this yet??
Right, then lets move on.
Now, the longer you take a medication the more your body gets used to it and the more that you may have to take to get that same therapeutic affect on the body and the pain that you are trying to manage. But, the more you have to take, the more dependent you become on that medication and the more worse you are going to feel when the medication wears off and tries to leave the body. Then it is going to take longer to ween off the medication, when you finally realise that you are dependent and that you need to so something about it. That is if you have that realisation, or finally admit there may be an issue.
One of the things that I have mentioned many times before, is that sometimes the body has been in pain that long, that the body doesn’t realise that it isn’t in pain any longer, that you also need to turn that response off, because it has actually become a habit, rather than the body actually still being in pain. The other issue is that the pain medications may in fact now be what are causing the pain, through rebound symptoms and withdrawal. This one is a bit tricky to explain to people, but in essence what we need to do is actually tell the body it isn’t in pain any longer, so that it switches off that response in the brain. To do that we need to detox an individual and then see what pain really does exist still and then manage those remaining symptoms. I will talk about proper medical detox further in the post.
Now let’s look at how pain medications, opiates and some elicit drugs work
Pain medications, Opiates and other pain relieving drugs, all change the way the brain responds to pain and they can also produce a “high” feeling by disrupting the reward and pleasure centres in the brain. This is why they can make you feel a bit stoned, or a bit light headed and why you should not drive, or operate machinery etc, while you are taking them. They can dehydrate and constipate you too, so this is why you should only take as directed and also make sure you drink enough water, take some electrolytes and take it easy too. Let’s not forget the serious side effects of medications that can put overload on your liver and other vital organs and actually shut them down, if taken for long enough, or in a super high dose.
The central nervous system, which includes the brain, cardiovascular and respiratory systems, has opioid and pain medication receptors that receive opiate drugs and other pain medications, and these drugs bring a variety of physical and emotional effects. Your heart rate, respiration, blood pressure, and body temperature are usually all lowered while pleasant feelings are increased. It can cause the opposite effect too, where some people get hyper-activated responses too.
Repeated use, or abuse, of pain medications, or an opioid drug, can actually change the way an individual’s brain chemistry works and then lead to physical and psychological dependence. The body may not feel “normal” anymore without the drug’s interaction, and withdrawal symptoms may start in between doses or when an individual stops taking the pain medication, or drug they are on.
What Are Pain Medication, Drugs and Opiate Withdrawal Symptoms?
Certain over the counter medications (such as codeine based meds), prescription painkillers, Opiates and heroin, can produce withdrawal symptoms just hours after the last dose, and the symptoms can last for a week or more. Sometimes these symptoms can be minor, but many times they can cause all manner of symptoms, which I will list below in detail. Some symptoms can be major and unassisted withdrawal may, or may not be life-threatening. When someone doesn’t withdraw properly it can also lead to relapse and further dependence on a medication, or drug. Medications and therapy, accessed in medical detox, may make relapse less likely. I’ll talk about why it is necessary to do a proper medical detox first, before seeing practitioners outside the medical detox model.
What Are Pain Medication ad Drug Dependency Symptoms?
Pain medication and drug withdrawal symptoms can last about a week, or even longer for some, and may include:
- Irritability
- Agitation
- Depression
- Muscles aches
- Insomnia
- Thoughts of suicide
- Anxiety
- Inability to concentrate
- Diarrhea
- Bowel Pain and Rectal Pressure
- Severe bloating
- Fluid Retention
- Sweating
- Body aches
- Runny nose
- Headaches
- High blood pressure
- Irregular heartbeat
- Many other symptoms not mentioned here
Detox and Withdrawal Duration
Withdrawal is the collection of side effects that occur when a drug is removed from the brain and body of someone who is dependent on it, while detox is the actual removal of the drug itself.
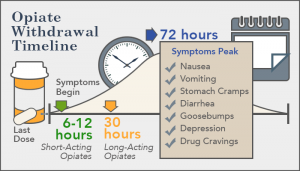
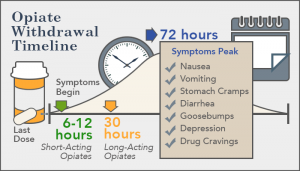
Withdrawal symptoms can last anywhere from a couple of days to up to a week or longer. For most pain medications and prescription opiates, withdrawal symptoms take shape 8-12 hours after the last dose and it peaks in the first 72 hours. The time within the withdrawal period depends on the medication, or drug taken. This is where rebound symptoms can occur.
The first week of withdrawal is typically the worst, but some symptoms may actually last longer. Symptoms typically last up to one month, but can linger for several months. Some effects can be permanent if there is a genuine abuse of a medication. Symptoms that can last longer than one week include tiredness, muscles aches and tiredness, depression, anxiety, and trouble with sleeping.
This diagram shows the withdrawal of these medications and time frames of side effects from withdrawal after the last dose is taken.
Medical Detox
Detox may begin before withdrawal symptoms start and while the drug is still active in the body. This way the drug can be safely removed. During medical detox, individuals are monitored around the clock for 5-7 days, vital signs are continually checked, and medications may be used to control more difficult withdrawal symptoms. If an individual is heavily dependent on pain medications, opiates, or took large amounts of the drug for a long time, or has a family or personal history of addiction, medical detox may last up to 10 days. Medical detox ensures that an individual is stable before moving on with a comprehensive substance dependence treatment and management program.
Relapse after a proper detox can increase the risk for a potentially life-threatening overdose since the brain and body may not be used to the same amount of drugs that was used before. Each year around 30,000 people worldwide die each year as the result of a prescription pain reliever overdose. Each year around 500,000 people worldwide seek emergency department treatment for a reaction to the abuse, or dependency of pain medications or drugs to help with pain. By decreasing pain medication side effects and dependency on these medications as drugs, an individual may be less prone to seek out these same pain medications and drugs again after detox. Medical detox can help sustain abstinence and potentially prevent a tragic, relapse-related consequence.
While there are non-medical forms of detox, I wouldn’t recommend someone doing these until a proper medical detox is done. Proper support and around the clock care is needed in the initial stages of a proper detox and this really cannot be provided out in private practice, or by complementary medicine practitioners during this initial stage. I am all for people seeing natural medicine practitioners and using natural medicines but this needs to be done after the initial medical detox. That first phase needs 24-hour care, medicines, psychological care and so many things that would be really hard to find out in a non-medical environment. There are some specialised centres that use a multimodality approach, using medical science and complementary medicines, but these are few and not always cheap to access either.
Sure, after the initial medical side of things, go your hardest and you should be seeking natural alternatives to pain medications and looking and diet and lifestyle choices to help deal with pain. You should also be seeking alternatives to pain medications and seeking therapies that can help manage your pain, such as acupuncture, herbal medicines, pilates, yoga, counselling etc. All these things are important for ongoing care and helping deal with disease states and ongoing pain. But if you have reached the point where you are dependent on a medication, or drug, you are going to need lots of help and you will need help with proper detox first. Please, do not think that those packet over the counter detoxes from a chemist etc, are a proper detox. They are just a herbal laxative that cleans out your bowel. Always speak to a qualified professional to get proper advice about detox and microbiome restore.
Having lived with pain and having actually properly detoxed off meds years ago, it wasn’t until I was off all meds and things managed properly while detoxing, that I realised that some of my daily pain, was actually withdrawal effect of my pain meds. I don’t think many people realise that this happens and all the nausea and migraines and headaches and increased pain, is actually withdrawal. Only once pain is managed well, a proper medical detox done and then a plan put in place, do people realise how much the meds were actually part of their daily struggle and it was all withdrawal. Then you can use proper pain management strategies and alternatives for pain and also preventative strategies too.
I hope this has given you all a better insight into pain, pain medications and withdrawal symptoms and if you aren’t being managed properly for your pain and pain condition, then you need to talk to your healthcare professional about this. Everyone’s pain and pain symptoms are going to be different, even if they have the same disease state, or inflammatory condition. This is why individual treatment plans are much more effective than a treating the masses approach.
I’ll do a separate post of some alternative to pain medications and drugs shortly, as it is whole post in itself. I will be collaborating with integrative medicine practitioner and mindfulness expert Rosa Bunn on this topic.
In the meantime have a read of my post about me knowing what it is like to live with pain
https://drandreworr.com.au/knowing-all-too-well-what-it-is-like-to-live-with-pain/
I have written quite a few articles on pain and pain management and I urge you all to have a read of them all, so that it gives you some understanding of where I am coming from and also some helpful pain management strategies
- https://drandreworr.com.au/getting-a-handle-on-pain-with-proper-pain-management/
- https://drandreworr.com.au/stop-telling-women-that-period-pain-is-normal/
- https://drandreworr.com.au/early-intervention-early-management-is-vital-for-gynaecological-conditions-menstrual-issues/
- https://drandreworr.com.au/period-pain-is-not-normal-and-doctors-in-australia-and-the-rest-of-the-world-need-to-start-listening/
- https://drandreworr.com.au/asking-the-right-questions-about-period-pain-gynaecological-issues/
- https://www.sciencedaily.com/releases/2017/06/170618103517.htm
- https://www.medicalnewstoday.com/articles/318532.php
Take care and if you do need help with pain and pain management and getting of pain medications, you can always come and see me and book in a proper consultation and I can help you and point you in the right direction too. Sometimes we all need a little help in the right direction and sometimes the first step is admitting you have a problem in the first place. Oh, yes, I also get that many of you have been missed and dismissed also and this is why you are where you are now.
Telling it how it is and keeping it real. I get it and I understand.
Regards
Andrew Orr
Master of Reproductive Medicine & Women’s Health Medicine
-No Stone Left Unturned