Category Archives: Pregnancy
Pre-Fertility Program Meet and Greet Appointment with Dr Andrew Orr
Dr Andrew Orr’s clinic has a Pre-Fertility Program “Meet and Greet” appointment available for those thinking of joining the Fertility Program and who just want to meet Dr Orr first and find out a bit more about the program.
The “meet and greet” appointments gives couples, or individuals, a chance to meet and greet with Dr Orr and have a quick look over their basic health history, as well as have the program explained to them. Patients can go straight on the program and bypass the meet and greet if they wish to do so. For more details about the Fertility Program (click link)
Couples attending the meet and greet appointment are sent out the pre-fertility program questionnaire, and this must be sent back prior to the appointment. The appointments can be in person, or online for those living out of our local area, or who are international. You will be given more comprehensive questionnaires upon signing up to the program.
Please note that the introductory meet and greet appointment is ‘half an hour only’ and ‘is not’ the initial consultation for Dr Andrew Orr’s Fertility Program. This means that you will not receive any medicinals, healthcare advice or referrals during this appointment. Please also note that Medicare and private health rebates are not available for this appointment. (The cost of the appointment is $120).
Dr Andrew Orr’s fertility program has assisted and in helping over 12,500 babies into the world and this number is increasing every week. He has helped couples locally, interstate and internationally and has had many media stories about his success with couples.
Dr Andrew Orr has been awarded a Masters of Reproductive Medicine and a Masters of Women’s Health Medicine through the faculty of medicine at University of New South Wales (UNSW). He is also a Doctor of Traditional Chinese Medicine, a Nutritionist, a Natural Medicine practitioner, a qualified Chef and more.
Dr Andrew Orr has a special interest in Fertility and Reproductive issues. With his wide range of qualifications and over 20 years experience in assisting reproductive and women’s health issues, he is able to bring you a truly integrative multi-modality approach to assisting couples with fertility and having a baby. His motto is “No Stone Left Unturned” and the media have named him “The Brisbane Baby Maker”
If you aren’t getting the answers you need and the help you need, then Dr Orr’s Fertility Program could just be the answer you are looking for. The Meet and Greet appointments allow you to see if this program will be what you would like to do. If you would like more information about this, please do not hesitate to call Dr Orr’s clinic, ask us to email you an information pack.
We look forward to helping you on your journey to have a baby, just as we have assisted over 12,500 (plus) couples bring their babies into the world too.
Regards
Andrew Orr
-No Stone Left Unturned
-The International Fertility Experts
Endometriosis Facts
Many things you have heard about period pain and endometriosis are wrong. These are the facts about Endometriosis
Regards
Andrew Orr
-No Stone Left Unturned
-The Endometriosis Experts
The Myth of The Barren Woman Runs Deep
The word “Barren” comes originates from the French word ‘Brehaigne’, which means not producing, incapable of producing offspring, infertility, infertile; sterile.
Sounds terrible doesn’t it?
Fortunately very few women are ‘sterile’ and the word “infertility” is often misused in our modern society. Nobody is truly infertile, unless they actually have reproductive organs missing, or have genetic abnormalities that will actually prevent conception from happening etc. When a couple is having trouble conceiving, we should really use the word “sub-fertility” instead of “infertility”
The problem with talking fertility, sub-fertility, or infertility is that we often reference, target, or even blame the woman. Yes, women are often the blame of not being able to conceive a child and therefore the myth of the barren woman still runs deep and is very much in existence and kept alive by all concerned today in our modern world.
But is conception and the ability to conceive a child inherently the fault, or responsibility of the woman?
The answer to that is “No!”, but there is still this expectation, or focus, that not being able to conceive all falls back on a woman. Sometimes women actually wrongly blame themselves, or wrongly take on that responsibility too. Some women will even take on that burden, to protect a partner, who may actually be the main issue.
Then we now have an area of medicine that has its focus as being the woman, because women are the primary driving force for wanting to have a child. Hence the vicious cycle continues in this terrible loop and then many, practitioners included, buy into the myth of the barren woman and so the cycle continues over and over again.
Well, I am here to tell you that women are not the only part of having a child and that men play just as big a part when it comes to fertility issues and not being able to conceive.
No matter what you get sold, or what BS (bullshit) you are sold, while pulling on your ‘I need a baby heartstrings’, to make you part with your hard earned money, the fact remains, and will always remain, that it takes a sperm and an egg to make a baby. That is basic biology 101 and no matter what someone tries to tell you, sperm quality is just as important as egg quality in this equation.
Every day I see practitioners, both medical and in complementary medicine, focussing in on women as the primary focus of fertility and actually feeding the myth of the barren women by their very actions.
Many times the men are overlooked, or ignored, or completely disregarded in the fertility equation. Not only is this unethical, to just treat and focus on the women when it comes to fertility treatment, but it is highly negligent as well. Men are not born with an inherent right to automatically be able to conceive and worse still, the male sperm levels have fallen by as much as 60% in the last 70 years, with sperm quality levels said to be dropping at an alarming rate.
So why is the focus, the burden, the guilt and the whole emotional baby roller coaster left solely to women?
Well, I have explained that practitioners are to blame, the fertility profession is to blame, society is to blame, guilt is to blame and last of all men are a big part of the issue too.
Men are often to reluctant passengers in the fertility journey and are often very happy to bury their heads in the sand and pass the responsibility of not being able to conceive onto a woman. Then many men are told their sperm is fine, when in fact it is far from being fine.
Over 50% of fertility issues are related to male factors and up to 85% of miscarriage issues may be related to male chromosomal, or DNA issues related to sperm. As I said before, research has now shown that the male sperm quality has fallen by up to 60% over the last 70 years and is actually on the decline. Men are often the bigger part of the fertility picture and it isn’t just the woman at all.
Semen analysis parameters are based on what is needed for Assisted Reproduction (IVF, IUI, ICSI) , not based on what is needed for natural conception and this is where some of the biggest issues lay.
Misinterpretation of semen analysis and misinterpretation of parameters have many men believing they have OK sperm, when in fact it is far from being OK. With modern procedures such as ICSI, we only need a few single sperm to be able to fertilise eggs and this can still be considered ok, because at least there was some sperm to fertilise the egg in the first place.
A few single sperm, or a few hundred sperm, or even a few thousand sperm is not OK when it comes to natural conception. We actually need a few hundred million sperm for it to be OK and even then they need to be motile and they need to be swimming properly (rapid progressive) and actually be of good shape (morphology)
While a semen analysis is often the first part of male fertility evaluation, it is also very limited. While we can look at morphology, motility, concentration, count etc, it does not tell us about the actual quality of the sperm inside. Many sperm may look ‘OK’ via a semen analysis, but inside their DNA integrity is poor and there are high amounts of DNA fragmentation and this can only be measured by a DNA fragmentation analysis. Even then, each time a man ejaculates, the quality of the sperm will be different and can differ by up to 20% in each ejaculate.
We also know that what a man eats, drinks and even his physical and emotional health will affect his sperm quality and that a man’s physical, dietary and emotional health can be passed onto his offspring through the sperm. This is why it is important for a man to get his physical and dietary and emotional health in check way before he tries to conceive a child with his partner.
We always say that the healthier a man is, the healthier his sperm is and the healthier the woman is, the healthier her eggs will be also. A healthy man and a health woman produce healthy babies.
I have been assisting couples with fertility and pregnancy for over 20 plus years now, and helped over 12,500 plus babies into the world, and I can tell you that conception is not just about the woman. It gets back to basic biology 101 that it takes a sperm and an egg to have a baby.
Even when couples are having issues trying to conceive, or doing IVF, or however they are trying to conceive, there will be some issue on the man’s side and the woman’s side. Unless there is absolute infertility on one side, or the other, there will always be a bit of both the man and woman to work on to assist in being able to conceive.
While the myth of the barren woman runs deep in society, fertility clinics and through the guilt handed down from their fellow sisters and mothers, fertility issues and the right to be able to conceive ‘does not’ fall solely into the hands of a woman, far from it.
Men are an equal part in the fertility equation and men need be held just as accountable when it comes to trying to have a baby, or if there are difficulties in conceiving.
No matter what anyone tells you, a man needs to be part of treatment, management and support of the journey to have a baby. This is a big part in my multi-modality fertility program.
Fertility isn’t just the responsibility of the woman, it is the responsibility of the man as well and I make sure both the man and the woman are properly investigated, clinically managed and helped with treatments as well.
If you do need help with having a baby, then please give my friendly staff a call and find out how my fertility program may be able to assist you
Regards
Andrew Orr
-Master of Reproductive Medicine (MRepMed)
-No Stone Left Unturned
-The International Fertility Experts
Eat nuts to help men’s … NUTS
Men, it is time to eat more nuts, to help your…. ummm… NUTS!
But this isn’t just about your family jewels, this is about helping with what they produce and helping you carry on your family tree. A diet rich in nuts has been shown to improve sperm count, motility, morphology and sperm DNA.
Recent research published in the European Society of Human Reproduction and Embryology (July 4th 2018) has shown the men that regularly eat nuts have improved sperm quality and function and less DNA fragmentation in their sperm.
In many forms of traditional medicines, foods and the shapes of foods, often correlate to an organ in the human body. To give you an example, walnuts look like a lung and they also look like a brain. There are now research papers to show that walnuts may assist with brain function and help with lung function as well.
Many of the foods we eat may also assist fertility. Many of these foods may look like a reproductive organ, or contain seeds in them. Fruits such as dragon fruit and kiwi fruit look like the shape of a testicle, or an ovary and have seed in them, which traditional medicines often say are good for the seed (meaning eggs and sperm on a fertility level)
Hence it is no surprise that nuts, can help with… ummm… well…. a man’s nuts (reproductive organs)
This new research showed that the inclusion of mixed nuts (almonds, hazelnuts and walnuts) in a regular diet significantly improves the quality and function of human sperm, according to results of a randomized trial which measured conventional semen parameters and molecular changes over a 14-week study period. The findings, say the investigators, ‘support a beneficial role for chronic nut consumption in sperm quality’ and reflect a research need for further male-specific dietary recommendations.
Results firstly found significantly higher levels of sperm count, vitality, motility and morphology in the men randomised to the 60 g/day nut diet than in those following their usual diets free of nuts. Moreover, the subjects in the nut group also showed a significant reduction in their levels of sperm DNA fragmentation, a parameter closely associated with male infertility. Indeed, it was this change in the level of DNA fragmentation in the sperm cells by which the investigators explained, at least in part, the improvement in sperm count, motility and morphology.
Nuts are dense foods containing many antioxidants, omega 3 oils, amino acids and folate. This may explain why nuts are so beneficial to improving sperm quality overall. Antioxidants help with oxidative stress, which can be a big factor in DNA damage to sperm and poor sperm quality. Antioxidants and amino acids help with proper formation of sperm at the cellular stage and help prevent damage to sperm cells and help with repair and formation of the DNA of sperm as well.
There is much more growing evidence through research literature that healthy lifestyle changes such as following a healthy dietary pattern can assist conception. Healthy parents make healthy babies. It takes a sperm and an egg to make a baby and healthy men produce healthy sperm. This is why it is important for not only the woman to be healthy prior to conception, but for the man to be healthy as well. The health of the father is passed onto the child and there is growing evidence to support this now.
When it comes to fertility and trying to have a baby, males need to be an equal part of the equation. Fertility isn’t just a woman’s responsibility and fertility issues are not just related to women.
Regards
Andrew Orr
-No Stone Left Unturned
-Women’s and Men’s Health Advocate
Story Source:
European Society of Human Reproduction and Embryology. “A diet rich in nuts improves sperm count and motility: Improvements associated with better male fertility and explained by a reduction in sperm DNA fragmentation.”
Sex During Pregnancy
It is completely safe for a woman to continue having sex throughout her pregnancy unless her doctor, specialist, or midwife has told her otherwise. Not only is it completely safe to have sex during pregnancy, but having sex can have some benefits also.
In my line of work, I see lots of beautiful pregnant bellies. It is so nice to see all those pregnant bellies and some I have been a big part in assisting them being able to fall pregnant.
Personally I think women look their best when they are pregnant. They look so radiant and beautiful and let’s face it, everyone loves to see a pregnant belly and comment how beautiful the mum to be looks. I am sure some women may not feel that way on the inside, but I can tell you that women do get that glow and radiance when they are with child.
When a couple first gets the good news about being pregnant.one of the things I always get asked is “Can we still have sex during the pregnancy?”
The answer will always be “Of course you can”, unless there is something that may prevent that from happening. Always talk to your specialist, or midwife etc, if you have any concerns. To be honest, sex during the early stages of embryo growth can actually assist implantation and sex can also help with the increase blood supply to the endometrial lining, which then helps feed and nurture the growing embryo and then later, baby.
It is important for couples to know that sex will not harm the baby at any stage during a normal, healthy, uncomplicated pregnancy. Can I just tell the guys that the uterus (womb) is closed off by the cervix and no man’s penis is ever going to get through that, or in many cases even reach it. They wish they were that big …lol
A woman may not feel like having sex in the first trimester, due to morning sickness, or some early bleeding etc, but I often have to have a joke the males that they are the ones that may be saying “No” later on in the pregnancy. A woman’s sex drive may increase at certain stages of the pregnancy, and this is important for couples to be aware of.
Intimacy can also be a great time for the couple to bond and come closer together. Some men become even more attracted to their partner during pregnancy as the results of different hormones, pheromones and changes to body shape, such as increased breast size.
During pregnancy sex can have many benefits for both the male and female. It can have the following benefits
- It can help with early implantation and assisting the embryo to implant and grow
- It can bring a greater level of intimacy and bonding for the couple
- It can increase the libido of the couple
- Increased hormones and increased blood flow to the genitals can mean better orgasms for women.
- Sex can increase the couples immune system and also keep them fit and healthy
- Sex during pregnancy can increase endorphins which make a couple more happy
The only issues couples may face is that as the belly grows bigger, they may have to adopt certain positions that are more comfortable for the woman. A pregnant woman may be more comfortable where she is in positions where she can control the speed and depth of penetration. Lastly, oral sex is completely safe during pregnancy as well. If a couple has any concerns, as stated, always talk to your healthcare practitioner, specialist, or midwife.
Sex and labour
There have been many studies to show that vaginal sex during pregnancy has no increased risk of preterm labour, or premature birth. As mentioned before, if there are concerns, you can speak to your specialist, midwife, or doctor.
When trying to induce labour, sometimes a midwife, or specialist may recommend for you to have increased levels of sex to try and bring the labour on. Many people think it is about the prostaglandins in sperm, which can help ripen the cervix, but it is more about the female orgasm.
When a female orgasms, not only is there increased blood supply to the female genitals and uterus etc, but it also helps with hormone activation, such as oxytocin, which is known as the love hormone. But this hormone can help to activate labour at the time a woman is due. It won’t help activate labour any other time in the pregnancy though.
It is possible that sex and orgasm could induce Braxton-Hicks contractions late in pregnancy. Braxton-Hicks are mild contractions that many women experience towards the end of their pregnancy. However, these contractions do not mean that a woman is in labour, or close to being in labour, so they really are of no concern.
When you may need to avoid sex
As mentioned before your specialist, midwife, or doctor are the best people to advise you when to avoid sexual intercourse during her pregnancy. Always consult with your specialist, midwife, or doctor if you are worried about any abnormal signs during pregnancy.The main times that sex might need to be avoided are:
- There are problems with an incompetent cervix, or issues with early labour, or threatened miscarriage
- Any Bleeding, or unexplained vaginal bleeding
- Leaking amniotic fluid
- If a woman’s waters have broken
Sex after giving birth
This will depend on many things and usually a woman will know when she is ready to have sex again. All new mothers need time to heal and recover after giving birth, or after a C-section. Women can return to sexual activity whenever they feel they are ready to do so. Some women may not feel like sex for a while after the baby is born and partners need to be aware of this.
Just to recap
In most cases, sex is completely fine during pregnancy and poses no risk to the mother or baby. Pregnancy can be a time where the couple can enjoy more intimacy and bonding with increased sexual activity. Like I mentioned before the only thing to be aware of is that some positions might become more or less comfortable as the pregnancy progresses.
It is important for a couple to continue to have a healthy happy relationship during the pregnancy time and to continue to have a healthy sex life throughout the pregnancy as well.
Regards
Andrew Orr
-No Stone Left Unturned
-Women’s and Men’s Health Advocate
-The Women’s Health Experts
Mediterranean Style Diet May Help to Improve Pregnancy Rates for Couples Undergoing IVF and Assisted Reproduction.
New research published in Human Reproduction, has found that those who follow a “Mediterranean” style diet at least six months before assisted reproductive treatment have a significantly better chance of becoming pregnant and giving birth to a live baby than women who did not.
As part of my Fertility Program, one of the first things I talk to couples about is the importance of a healthy diet that has adequate protein, lots of vegetables, seeds and nuts, healthy oils, adequate water intake, electrolytes and cutting out all the refined carbohydrates that cause inflammation.
The hard thing is that I hardly see a couple following those health food principles, with many not even really knowing what a health diet is. The diet that I promote is based on my specially formulated PACE diet.
Previous studies have shown that when refined carbohydrates are cut out and replaced with proteins, essential fats and good carbohydrates, such as fruit and vegetables, that the clinical pregnancy rates shot up by 80%. (Fertility & Sterility 2012 Volume 98 issues 3 Page S47)
In this new study, researchers focussed in dietary patterns rather than individual nutrients, food, or food groups. They found that those who ate lean protein, more fresh vegetables, fruit, fish and olive oil, had a 70% greater likelihood of achieving a successful pregnancy and birth compared to women who didn’t follow this style of diet.
The research outcomes found that out of the 244 women in the study, 229 women (93.9%) had at least one embryo transferred to their wombs; 138 (56%) had a successful implantation; 104 (42.6%) achieved a clinical pregnancy (one that can be confirmed by ultrasound); and 99 (40.5%) gave birth to a live baby.
The most important message to come from the study is that women attempting to have a baby should be encouraged to eat a healthy diet, such as a Mediterranean style diet, because it may help increase the chances of successful pregnancy and successful live birth.
The researchers did note that when it comes to conceiving a baby, diet and lifestyle are just as important for men as for women. Previous studies from the same research group showed that male partners that adhered to the same sort had better semen quality.
A healthy diet is important for all couples prior to trying to conceive and should be a part of any preconception planning by all healthcare practitioners assisting couples with fertility.
While this study focussed on improving assisted reproduction pregnancy rates, this style of diet should be adopted by any couple wanting to have a baby and should be implemented at least 6 months prior to conceiving. This is why it is essential for all couples to receive counselling and guidance on the importance of a healthy diet and having a healthy lifestyle as well.
This is a foundation of my fertility program that has helped over 12,500 babies into the world and continues to assist many more couples reach their goal of becoming parents. If you would like to find out more about my fertility program and how it may assist you, please give my friendly clinic staff a call to find out more.
Regards
Andrew Orr
-No Stone Left Unturned
-The International Fertility Experts
Zinc Deficiency Affects Egg Quality and Early Stages of Egg Development
Recent studies have shown that zinc deficiency can negatively affect the early stages of egg development, reducing the ability of the egg cells to divide and be fertilised.
This may affect fertility “months” in the future and why preconception planning is so important for a couple. The researchers will be presenting their results at the American Physiological Society annual meeting at Experimental Biology 2018 in San Diego.
Millions of couples around the world struggle with fertility issues and the ability to conceive a child. While there are many factors that can make conception difficult, ovulation disorders and sperm issues are a leading cause of couples not being able to conceive. Researchers are finally looking into how vitamins, amino acids and micronutrients affect fertility and in particular the early stages of egg development.
The availability of micronutrients, through diet, amino acids, antioxidants and vitamin supplements, in the ovarian environment and their influence on the development, viability and quality of egg cells is now the focus of a growing area of research. Sperm also need micronutrients, antioxidants, vitamins and nutrients for optimal growth and development too.
This is nothing new to me as this is something I have always focussed on for many years as part my fertility program and as a part of preconception planning and making sure that the couple are in optimal health before trying to conceive.
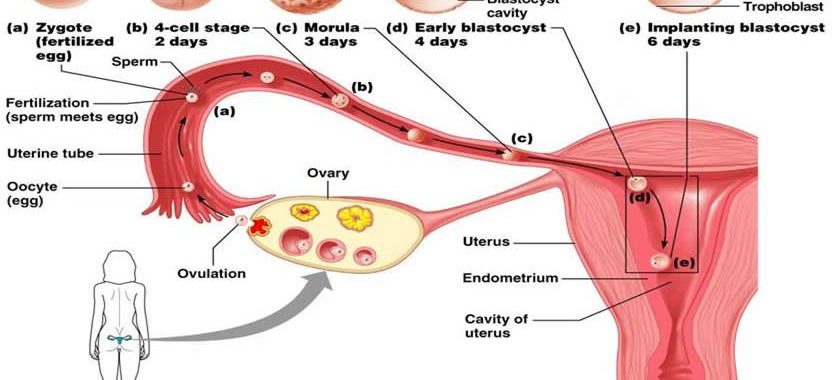
In human and mammals, the ovary is made up of thousands of structures called follicles, which consist of one oocyte surrounded by layers of support cells, known as somatic cells. At puberty, the body starts to prepare groups of oocytes for maturation, ovulation and fertilization. While a female grows groups of oocytes, which begin to mature each month, only one will be ovulated and have the chance of being fertilized. Many things can influence whether an oocyte will mature correctly and the go on to one day be ovulated, including the presence of sufficient levels of certain micronutrients. To date this has probably been poorly understood by many.
Scientists have recently found more and more evidence to show that zinc is a key player in oocyte development and have been assessing the effects of zinc on egg development extremely early on in the development and maturation of oocytes.
Previously Fertility research and treatment has primarily focused on the larger follicles, called antral follicles, which respond to signals from the pituitary gland to be ovulated.
In humans, preantral follicles have to keep growing for about 90 days before they are ready to ovulate. This is why it is important to focus on egg and sperm quality months before conception is to take place, because this is when both egg and sperm are still growing and maturing and need vital nutrients to develop properly.
In this new research they have examined the smaller preantral follicles, which are still growing and don’t respond to the ovulatory signal yet. Previous studies showed that zinc levels are critical in the antral follicle, but no one had tested the effect of zinc deficiency on preantral follicle growth.
The researchers collected preantral follicles and then matured them in a special cell culture medium. They compared eggs matured in a zinc deficient environment to those grown with normal levels of zinc. The researchers found that preantral zinc deficiency:
- Impaired the egg cell’s ability to properly divide (meiosis), which is a necessary step before successful fertilization can occur.
- Led to smaller and more immature egg cells early in development
- Hindered and disrupted growth of the cells
- Caused problems with development of somatic cells and elevated certain cell markers.
The new research shows that zinc plays an important role in oocyte growth at an earlier stage than previously investigated, which is during development and before division. The research also showed why preconception nutrients are needed months before the eggs fully develop to give the best outcomes for a healthy pregnancy.
It is estimated that about 17 percent of the global population may be deficient in zinc, due to poor dietary intake their diet. But the estimate may not include cases of marginal zinc deficiency, where people may be getting zinc in their diet, but not enough for their recommended levels.
People that are more susceptible to zinc deficiency are those with dietary and disease factors such as irritable bowel syndrome, Crohn’s disease, gastrointestinal disorders and liver disease, those with eating disorders, those with certain dietary restrictions, such as vegetarians or vegans, who may not then be taking supplemental zinc.
Preconception planning, care and management is so important for a healthy pregnancy to occur and should be started many months before trying to conceive. This is to ensure that the sperm are in optimal health and quality and also to make sure that the egg quality is optimal and in the best quality it can be as well.
This is what I do for all my fertility patients and is a crucial part of my fertility program that has now helped over 12,500 babies into the world. If you would like to find out more about my fertility program and how is may be able to assist you, please call my friendly clinic staff and they will be able to explain everything to you.
Regards
Andrew Orr
-No Stone Left Unturned
-The International Fertility Experts
A new male contraceptive compound can immobilise sperm temporarily without side effects
What is Bladder Endometriosis?
Endometriosis is a condition where tissue resembling the uterus lining grows outside the uterus, such as on the ovaries or fallopian tubes. Endometriosis can spread to every organ in the body and can grow inside, or on the outer surface of the bladder.This is what is known as Bladder Endometriosis.
To learn more about endometriosis and to learn about the symptoms of this disease, you can click on this link to find out more (Click Here)
If endometriosis forms in, or on the bladder, it that can cause severe discomfort and pain. It can also make a woman want to urinate more and also with urgency, pain, burning and frequency.
There are other bladder conditions with the same, or similar symptoms, but endometriosis can also aggravate these conditions, or be present at the same time as well. I will discuss the other forms of bladder pain and interstitial cystitis, which can have similar symptoms to endometriosis affecting the bladder, or bladder endometriosis.
Prevalence
Bladder endometriosis is not common. Reports state that around 2 percent of women with endometriosis may have endometrial growths in their urinary system, with endometriosis growing in, or on the bladder. But even if endometriosis isn’t on, or in the bladder, it can still cause issues with the bladder and cause associated symptoms.
What are the Symptoms of Endometriosis in, or on the bladder?
One of the main symptoms bladder endometriosis is pain when the bladder is full and a woman needing to urinate more frequently. It can also cause symptoms resembling a urinary tract infection, but no infection will be found to be present. Women do need to be aware that a significant portion of women with endometriosis are asymptomatic (meaning no symptoms) and may not be aware that they have endometriosis until they have investigations for another reason, such as not being able to fall pregnant.
Some women are more likely to notice symptoms of endometriosis around the time they are due to have their menstrual cycle.
Other symptoms of bladder endometriosis may include the following:
• More frequent need to urinate
• Needing to urinate urgently
• Feeling pain when the bladder is full
• Stinging and burning or painful sensations when passing urine
• Seeing blood in the urine
• Experiencing pelvic pain
• Having lower back pain, more on one side of the body
Diagnosis
The definitive diagnosis for endometriosis is via a laparoscopy as this is the gold standard investigation for investigating disease states inside the pelvic cavity. A biopsy is usually taken at the same time to check the microscopic implants of endometriosis, which cannot be seen visually. Normal ultrasound, transvaginal or abdominal, cannot diagnose endometriosis. Blood tests cannot diagnose endometriosis either.
If Endometriosis has spread inside the bladder a cystoscopy would be needed also. A cystoscopy is where a small scope is inserted into the bladder and the specialist can then see if there is endometriosis, or other inflammatory disease in the bladder lining.
The specialist will then see what stage the endometriosis is at. This is a staging system from 1-4, but this is only to let the surgeon know how much of the disease is present. The staging system does not have anything to do with pain levels, as pain levels “are not” related to the extent of the disease. A woman with stage 1 endometriosis could have more pain than someone who is stage 4, and someone who is stage 4, may not have any pain, or associated symptoms at all.
Treatment
There is no current cure for endometriosis. However, the condition can be managed through a multimodality approach that involves surgery, hormones, pain medication, physiotherapy, herbal medicines, acupuncture, yoga, pilates, diet, lifestyle changes, counselling and an individualised approach. Women with endometriosis need a team approach.
Surgery, via a laparoscopy, is the most common treatment, and definitive diagnosis, for those with endometriosis. If endometriosis had been found in the bladder transurethral surgery will be done at the same time. This involves a scope inside the bladder to cut away any endometriosis in the bladder lining. Sometimes a partial cystectomy is needed to remove an affected part of the bladder.
While surgery is a much-needed part of the treatment and diagnosis of endometriosis, it is not a cure. Endometriosis can, and often does, grow back again, even with the best medical forms of treatments and interventions.
Fertility
Bladder endometriosis does not have any effect on a woman’s fertility. However, endometriosis does grow in other parts of a woman’s body and reproductive system such as the ovaries, which may affect a woman’s likelihood of conception. But, endometriosis does not always affect fertility.
The Difference Between Bladder endometriosis interstitial cystitis
When endometriosis gets in the bladder it can cause very similar symptoms to another bladder condition called interstitial cystitis. This can often make it very hard to differentiate on symptoms alone.
It is also very possible to have both interstitial cystitis and endometriosis present at the same. This is why further investigations are needed to definitively diagnose both these conditions.
I do have a separate post on interstitial cystitis so that people know more about this inflammatory condition that affects the bladder.
Outlook for Women With Bladder Endometriosis
At present there is no real known cause of endometriosis and only speculation as to what the true cause is. We know that endometriosis is estrogen driven (not from estrogen dominance), but the most likely cause is probably due to genetic reasons and being a hereditary condition passed on through the parental mode of inheritance and then expressed into the body. The how, when and why will hopefully be answered in the not too distant future hopefully.
Women with endometriosis in the bladder do need to be careful and managed properly as it can cause kidney damage. There is also some research to show that endometriosis in the bladder can lead to cancer in the bladder, but this is thought to be very rare.
For now, anyone with endometriosis needs to be clinically managed properly through a multimodality team approach mentioned before. Let’s get more education out there so that women with this horrible disease have a voice and we end the silence for these women as well. Hopefully through education, funding and further research, this leads to the cure that women with endometriosis so desperately deserve.
If you do need help with endometriosis, please call my clinic staff and find out how I may be able to assist you. I do have a special interest in endometriosis and am very passionate about women receiving the right care and health management moving forward.
Regards
Andrew Orr
-No Stone Left Unturned
-Period Pain IS NOT Normal
-The Endometriosis Experts