We have not long gotten over the Christmas and New Year period and we are about to embark on the fast train into Easter holiday and festive season.
While many are getting ready for the sugar fest ahead, with Easter eggs and hot cross buns galore, we need to take the time to understand how this may affect our bodies afterwards, especially for women and their menstrual cycles.
Worse still it could even affect pre-existing gynaecological conditions that women live with on a day to day basis, some of which impact women’s day life terribly.
Christmas and Easter times always pose great problems for women and their menstrual cycle, and year after year many women never make the correlation why.
Year after year I see women coming back to see me, after Christmas and Easter, scratching their heads as to why all of a sudden their menstrual cycle has gone haywire and they are getting the worst PMS symptoms they’ve had since they can remember.
So why do so many women have problems with their menstrual cycle after Christmas and Easter?
The answer is blatantly obvious. Stress, Poor diet and Lifestyle factors!
The lead up to Christmas and Easter, is always a busy time and no matter how much people try to deny it, it is very stressful. People are rushing madly to meet deadlines before everyone goes on holidays and then the mad Christmas and Easter shopping rush that follows.
Then there is the stress of what to buy everyone, followed by the mad catering panic. People literally go mad and one would think the end of the world is imminent, with supermarkets being emptied by the marketing hype of these two festive seasons.
Then the big day arrives. Everyone forgets the basic principles of a healthy diet and engorge themselves on any food they can lay their hands on. Basically it is a licence to eat as much bad food as we can put in our mouths, and then use the basic excuse of “Its Christmas” or “It’s Easter” and “It is only just one day and it won’t really matter and I had to do it”.
Then one day leads into two, and then this leads into a week and then before we know it, it has been more than just one day of bad eating, or drinking alcohol. The sad fact of that statement is that some people eat and drink alcohol like it’s Christmas and Easter every day.
With Christmas we can have many portions of baked dinner, crackling, seafood, Christmas pudding, chocolate and any other sugar substance that can be consumed it all had to be washed down with a nice alcoholic beverage, or two. Many bottles of bubbly, or choice of poison later, and we now have a stomach full of sugar, fat, cholesterol and alcohol all churning quite nicely. Diabetes and heart disease here we come.
Then approximately 1 week later it is New Years Eve and the license, to drink like fish and eat like a ravenous bear, is pulled from the pocket and waived around once more. “But it’s Ok”, we say.
The New Year’s resolution will be to not do it again, until next year when all resolutions are forgotten. Meanwhile the system had short circuited, the gut has gone into melt down, the cholesterol levels are rising, the sugar levels have reached diabetes status and the brain cells have been reduced yet again.
Several months later when the system has started to recover, Easter arrives and the sugar binge begins; with Easter eggs and all manner of chocolate, sugar laden delight. Let’s not forget the alcohol added to the mix, that we used to self medicate from the stress of the lead up to the Easter break. The body short circuits itself again and will take until Christmas to recover and then it starts all over again.
Now, I wonder why the menstrual cycle would be affected?
Hmmm, I wonder?
There are only a few things that will affect a menstrual cycle and cause PMS, irregularities and pain. The trouble is many of them can be unknowingly self- inflicted. Yes, many monthly menstrual related problems can be unknowingly self- inflicted.
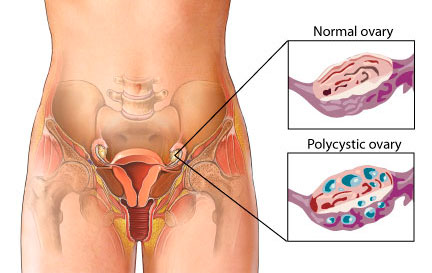
Let’s not forget that many people do have gynaecological issues that they suffer on a daily basis though. But even still, this high amount of burden on the system will exacerbate these pre-existing conditions and make them worse, due to the resulting high levels of inflammation.
What I am trying to do is just make people aware of how conditions can be worsened and how these high levels of inflammation, from high levels of sugars etc, can cause havoc with a woman’s cycle. This is not about blame. It is about education and prevention. I am here to help, not hinder. Please remember this.
As I said there are only a few things that affect, or exacerbate, a woman’s menstrual cycle and I’m going to list them below. So that way if you are wondering why you can’t get enough Naprogesic into your body, when you get your cycle, please remember the list below.
Please also read my article on “What a proper Menstrual Cycle Should Be Like”. If it isn’t like the one I describe you better book in to see me soon.
What Affects a Menstrual Cycle
- Poor diet – Foods such as high sugars and junk foods all cause inflammation in the body and lead to hormonal irregularities and pain with the menses
- Alcohol – Most alcohols contain high sugars and they also cause inflammation in the body. It also interferes with your hormones and affects the liver too. In Chinese medicine the Liver governs the menstrual cycle. Excess alcohol leads to SOL ( Shit on Liver)
- Poor Sleep– Sleep deprivation leads to reduction in hormones such as serotonin and then effect the moods etc. Lack of sleep also stops the body from repairing and can lead to other health issues
- Trauma – Things such as surgery, a virus, cold/flu etc, or where the body has to repair, can lead to menstrual irregularities. The body shuts down the menses so that it can repair itself first
- Weight gain or weight loss– It is a well known fact that many athletes do not get a menstrual cycle because of lack of body fat. The same goes for people who are overweight too. Too much, or too little, body fat interferes with your fertility. All your hormones are made from fats and protein.
- Emotional Issues– Bottled up emotions such as anger & frustration cause blockages in the system & then cause pain. Emotional issues, such as anxiety also cause problems with hormones and lead to further pain and inflammation. Emotions can be a major issue in any health condition, or can affect hormones.
What a proper menstrual cycle should be like
A proper menstrual cycle should be 26 –32 days in it’s length. It should be 4 days flow, 5 at the most. Any shorter than 4 days is too short and any longer than 5 days is too long. This isn’t good.
You shouldn’t get any pain at all, you shouldn’t get clotting, spotting, breast tenderness, bloating, fluid retention or changes to the moods such as teariness or irritability. These are all signs of irregularities that may need to be addressed.
Some of the things that exacerbate menstrual issues are listed above.
Lastly, please know that Period Pain IS NOT Normal and neither are some of the other irregularities women have. If you are suffering pain, or irregular cycles, or any other issue that doesn’t seem right to you, you need to get it checked out.
If you would like to book in a consultation with me, please call my friendly staff, or using the automated emails system on the website.
Regards
Andrew Orr
-Master of Women’s Health Medicine
-“Leaving No Stone Left Unturned”
-“Period Pain IS NOT Normal”
-The Women’s Health Experts
-The Experts Program