In today’s modern society, alcohol has become the cornerstone for social engagements, business dinners and after work relaxation. It is important to realise however, that alcohol can directly impact the fertility of both males and females.
In males it can decrease sperm quality, reduce testicular size, decrease libido and cause impotence, all of which can impair fertility.
In females it has a more systemic response, affecting the reproductive hormones, leading to abnormalities in the menstrual cycle and an increased risk of miscarriage.
Many men and women these days are actually consuming copious amounts of alcohol and may think that their drinking habits are normal, when compared to others around them.
When people do things on a regular basis, it becomes their normal. But truth be told, many people’s drinking habits, both men and women, are actually in the realms of alcoholism. The impacts of that are far reaching and fertility and gynaecological conditions are definitely impacted by alcohol consumption.
Effect of Alcohol on Conception for Men
Fecundability refers to the probability of conception during a particular menstrual cycle. It is dependent on the reproductive potential of both partners. Alcohol decreases fecundability by its effect on sperm quality and quantity. Men who continue to consume alcohol on a regular basis, can decrease their sperm motility, morphology and their DNA in the sperm. All of which are important factors in achieving fertility.
While outwardly a man’s sperm may look OK, many forget that inwardly, the sperm DNA could be highly fragmented and unless this is tested every ejaculation, you will have no idea how bad the sperm actually is. A one off DNA fragmentation analysis does not mean the sperm each time is OK. It only measures the sperm from the ejaculate that was tested and sperm quality can change by as much as 20% each ejaculation.
Testicular size is also affected by alcohol intake; and can also affect sperm production. Alcohol is a depressant of the central nervous system (CNS), and can disrupt the autonomic system of the CNS. These effects are temporary and short lived. Abnormal sperm production is also temporary and also can resume after abstaining from alcohol.
One study, this one looking at couples going through IVF treatment, found that for every additional drink a man consumed per day, the risk of conception not leading to a live birth increased by 2 to 8 times. This was especially true if the drinking occurred within a month of the IVF treatment.
Effect of Alcohol on Conception for Women
In women, alcohol affects fecundability, by disrupting the delicate balance of the menstrual cycle. Clinical research data published in the “British Medical Journal” suggests that women, who drank socially, 1-5 drinks per week, were at a greater risk of decreased fecundability when compared to women who remained abstinent. These findings underscore the importance of remaining abstinent while attempting to conceive.
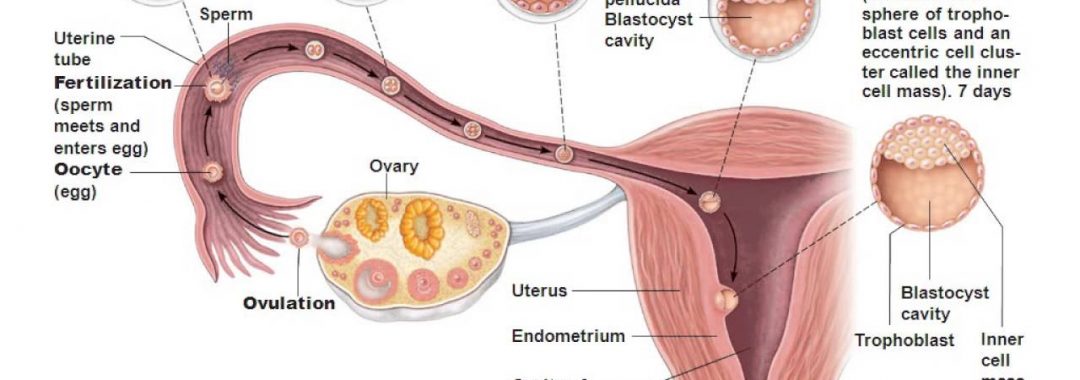
Alcohol disrupts the hormonal imbalance of the female reproductive system, leading to menstrual irregularities, and even Anovulatory cycles, (menstrual cycles where ovulation fails to occur). Menstrual pain can directly be linked to the amount of alcohol consumed in the lead up to the menses and consumptions of alcohol, even small amounts, exacerbates most gynaecological conditions. These changes can drastically decrease a woman’s chance of becoming pregnant and thus affect fertility.
Alcohol effects fertility in both partners, and can do so in so many ways. For couples who desire to have a baby, it is best to stay away from drinking completely. Presently there is no safe limit of alcohol intake; even socially acceptable amounts of alcohol can affect fertility potential and outcomes.
Moderate drinking (1-2 drinks in one sitting) is probably okay, especially if you reserve those drinks to a few times a week, instead of daily. However, if you’re going through IVF treatment, or trying to conceive naturally, you might consider cutting out alcohol for the time being.
A woman that is trying to concieve, or trying to improve a gynaecological issues, or menstrual issues, should not be consuming more than 4 standard drinks per week.
A male who is trying to conceive, or have sperm quality issues, should have no more than 2 standard drinks in one sitting and be having at least 2 alcohol free days per week. These are all part of the healthy drinking set out in health department and government safe drinking guidelines.
Trying to conceive is a special time in a couple’s life, it should be filled with love, devotion and safe health practices, which means a healthy diet and lifestyle and having a healthy mind too. It also means having healthy drinking habits as well.
Decreasing alcohol, having bete foods and looking at a healthy detoxification program is also a great idea for those trying to increase their fertility and get their reproductive systems working better. Healthy eggs and health sperm make healthy babies. Healthy reproductive systems also mean better menstrual cycles and better testicular health too.
Safe drinking everyone. This is something I talk about as part of my fertility program and preconception care. If you would like to find out more about my fertility program, please contact my friendly staff to find out more.
Regards
Andrew Orr
-Women’s and Men’s Health Advocate
– No Stone Left Unturned
-The International Fertility Experts