My main aim is to bring awareness about Endometriosis also end the silence for sufferers of this disease that is often overlooked and often ‘missed’ and ‘dismissed’. It is an issue myself as an Endometriosis Expert feels very passionately about.
I help and care for women suffering from this disease every day and I hope that one day, endometriosis can be a word of the past. There is no cure for this disease, but we need to find one.
Through awareness and education, let’s try and get women the early intervention and help they need sooner, rather than later.
What is Endometriosis
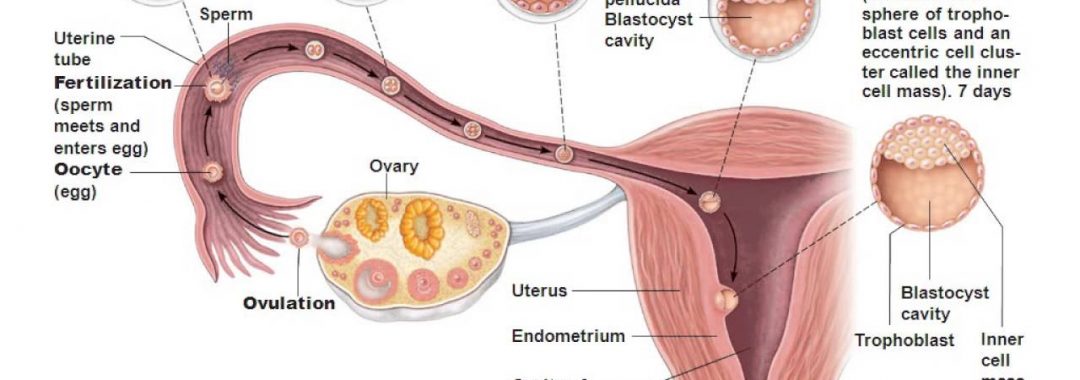
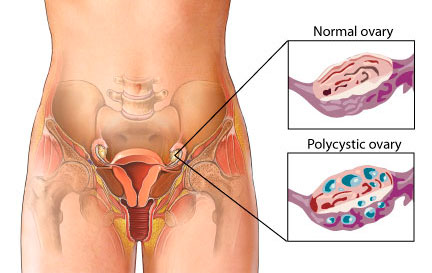
Endometriosis, which is an inflammatory gynaecological disease, by which endometrial like tissue grows outside the endometrium. It can spread outside the endometrium into the pelvis, bowel and intestines. It has even been known to get into the brain, joints and around the heart.This disease affects 1 in 10 women, often causing immense pain for them.
According to the Royal College of Obstetricians and Gynaecologist Guidelines for the Management of Endometriosis, it can cause the following symptoms:
Heavy Menstrual Bleeding
Period Pain
Pain with sex
Ovulation Pain
Irritable bowel like symptoms
Bladder issues
Chronic fatigue
Pain with bowel movement
The disease can also cause other symptoms such as :
Bloated belly that looks pregnant around your period (known as endo belly)
Bloated belly that looks pregnant and you are told it is from certain foods, but it isn’t, or may be a combination of food and inflammation from endometriosis (also known as endo belly)
UTI like symptoms that aren’t a UTI
Bleeding from the bowel with your period
Low Iron with no explanation
Being told you have IBS, but you don’t have IBS
Migraines/Headaches that are worse around your period
Irrational mood swings
There are so many other symptoms that could also be pointers to endometriosis.
This disease can also play major havoc with hormones and the libido. Many women with can have pain on intercourse which further lessens the desire around sex.
Women with endometriosis often have painful periods and can’t get out of bed, so if you experience this, there is a good chance that you actually have it.
Women with endometriosis can also have other hormonal disturbances such as mood swings, fatigue, restlessness etc. They can also have other symptoms such as migraines, headaches, dizziness, constipation, pain with bowel movements, joint pains and all manner of symptoms created from the inflammation that endometriosis is caused by and also creates
How Many Women Suffer from Endometriosis?
Endometriosis has now reached an all time high in its ever-growing presence. While the current research says that 1 in 10 women are affected by endometriosis, as an endometriosis expert, I believe, as do many others, that these figures may be grossly under exaggerated.
Research also shows that a significant portion of women affected with endometriosis are asymptomatic (no symptoms) and may only ever get diagnosed if they are having issues with having a baby, or they may never be diagnosed at all. In addition to this, many women diagnosed with Irritable Bowel Syndrome actually have endometriosis and not IBS.
Many women have also been told period pain is normal and hence many never seek help for a condition that can be debilitating on their life and those around them. Women who suffer period pain and other menstrual related symptoms caused by endometriosis are often ‘missed’ and ‘dismissed’ by multiple healthcare professionals and it can take up to 12 years from onset of symptoms to a definitive diagnosis being made.
Women with period pain caused by endometriosis have to live a life of pain, trauma and physical and emotional torment. Many of these women are barely getting through a day, let alone a whole month of exhausting symptoms related to this disease. Some sadly even turn to suicide.
The Western Medicine Approach on the Causation and Treatment of Endometriosis
To date, Western medicine does not know how or even why endometriosis occurs. New research is showing that the disease is a genetic disease that is hereditary.
The only solution that has been offered in the past was to laser it. This usually has a recurrence rate of up to 80%.
The proper way that this disease should be removed is by excising it (cutting it out), which offers better relief with less recurrence.
I do need to stress that when a surgeon is needed, it needs to be done by an advanced trained laparoscopic surgeon, who has had extra specialised training, and is an expert in endometriosis excision and management, and is not just any obstetrician/gynaecologist (OB/GYN). This is where many go wrong and haven’t had the disease dealt with properly.
Despite the increased success in treating endometriosis through a surgical procedure, it still usually reoccurs in a majority of women. There is no cure for endometriosis. To find out more about the facts about endometriosis please click on the link- The Facts About Endometriosis
So why isn’t the medical option alone working?
Primarily it is because they are just treating the symptoms and not the cause. You can take away most physical symptoms very easily, but if the real cause isn’t addressed at the same time, you have no chance of a full recovery. This includes emotional factors.
In addition, many of the hormones that women are put on after surgery, mask the problem and can actually make it worse. By actually stopping the the normal menses, like many of these hormones do, there can be increased risk of further endometriosis growing. Sure, while you have no period, you may have no pain or symptoms, but internally it is still there waiting to flare up again.
Oral contraceptive pills containing estrogen should be avoided as they only add to making the problem worse. Progesterone only options should be looked at rather than a combined pill, if using hormones. These treatments also have limitations that include side effects in some women and contraceptive action for women desiring to conceive.
The Traditional Chinese Medicine Approach on the Causation & Treatment of Endometriosis
Firstly, I can only pass on what the Chinese have known and studied for 10,000 or more years, much longer than western medicine. They had the body and its internal organs mapped out longer before medical science in the west did.
In Chinese Medicine, they believe the liver governs the menstrual cycle, and that it also governs our emotions.They believe that through poor diet, lifestyle, medicines, environment etc, that these can then cause disruption to an organ in the body. Emotions such as anger, frustration, resentment, stress, irritability etc, are believed to cause the liver to be in disharmony.
In Western Medicine terms, we know that poor diet and emotional factors can unlock predisposed hereditary issues, or dispositions through DNA recoding. Yes, diet can affect your DNA coding and so can emotional issues. Similarly we can reverse some disease states, and reprogram DNA coding through a healthy diet and fixing our emotional health.
When the liver is in disharmony, Chinese medicine believes it can cause blockages in our system. Western medicine now also believes that emotions can cause physical symptoms and we often see this is psychiatric, or body-mind medicine. These blockages then cause what we call stagnation.
Chinese medicine believes that when the Qi (energy) becomes stagnant, it causes what they call Liver Qi Stagnation, and this is the cause of many gynaecological conditions such as endometriosis and PMS.
Chinese Medicine believes that when Qi stagnation is left long term, it then affects the blood and turns it stagnant too. Imagine damming a river and the longer the water sits, the more stagnant it becomes because it no longer flows. This is where the term “Blood Stagnation” comes from and what Chinese Medicine believe endometriosis is manifested from.
When we look at endometriosis, it does present as blood clotting and pain. Basically it is like a varicose vein that has all that old, stagnant blood in it. The circulation is no longer moving and the blood now turns dark and causes pain.
Chinese medicine believes that not only is diet and herbal medicine needed to move the stagnant blood and help prevent the disease further expressing itself, but also believes that the emotional component behind it also needs to be addressed.
In Chinese medicine they use lots of warming and blood thinning herbs that are also anti-coagulants, but are also anti-spasmotics. The Chinese medicine also has herbs to help the liver function and also help with emotional wellbeing.
Dr Andrew Orr’s Recommended Approach to Treating Endometriosis
Endometriosis has a highly variable disease state, and thus a multi-modality approach is needed to treat it. Targeting different pathways is likely to be important to move toward precision health (personalised medicine) in endometriosis. People with endometriosis need a team of people looking after them, not just one person and one approach.
For severe cases you will need to see a good advanced laparoscopic surgeon to get as much of the endometriosis excised (cut out-not lasered). Surgery is a much needed option if the pain is severe because it helps removed the deposits (lesions) of the endometriosis that can be seen.
However, it does not deal with the microscopic implants of endometriosis that can’t be seen, and this is why endometriosis is likely to occur again. We do know that despite the best medical interventions that women who have endometriosis can still be in pain and endure the terrible associated symptoms of the disease as well.
Acupuncture and Chinese Medicine may be able to assist with endometriosis and the associated symptoms of this disease . There is now some good anecdotal evidence to suggest that Acupuncture and Chinese herbal medicine may assist with the causes of period pain. This should be done along side medical treatments as well.
To support my view on the treatment of endometriosis, the Royal College of Obstetricians and Gynaecologists guidelines for treating endometriosis now states that Acupuncture and Chinese Herbal Medicine may assist in the management of endometriosis and should be considered.
Following the correct diet and restoring good gut bacteria and gut health (the microbiome) may also help with inflammation and the associated gut related symptoms of endometriosis.
The modern Western diet consists of many foods with high GI levels, causing inflammation to the body and therefore fuelling conditions such as endometriosis. There are all sorts of diets out there attesting to be the cure for endometriosis, but half are them are actually making it worse. A low GI /Low inflammatory based diet may help with assisting the treatment and management of endometriosis and its associated symptoms.
Lastly, see a good counsellor. Different modalities may help both the physical & emotional side of many disease states, but sometimes solution-based talk therapy is needed for the best results.
I provide patients with a list of preferred counsellors and psychologists when I see them for their initial consultation. I always look at the emotional side of everyones health and wellbeing.
A multi modality approach does help, but for anything to work more effectively, you too, have to make a commitment. It is also about finding your team and the team of people right for you too.
Who I am and Why this Means so Much to Me
I am a healthcare practitioner with over 20 years of experience in assisting Women’s Health Medicine and helping women with care and managing endometriosis and its associated symptoms. I know all too well the trials and tribulations women have to go through before someone actually listens and gives these poor women a proper diagnosis.
I also have loved ones with this disease and have also lived with a chronic painful disease too. While I may not fully understand and feel what women with endometriosis actually goes through, I do know what it is like to live daily life with a painful chronic inflammatory disease that can rule your life on every level.
The one thing I do want all women to know is that “Period pain IS NOT normal” and all too often women are told that period pain is normal. Nothing could be further from the truth. We need to educate women and young girls that period pain is not normal.
I have a motto of “Leaving No Stone Left Unturned” and I apply this to every patient I see with period pain, and those potentially suffering from endometriosis.
I would like to see better education and awareness for the general public, but I would also like better education and awareness for healthcare professionals. I would like to see all healthcare professional use my motto and make sure that no woman is ever ‘missed’, or ‘dismissed’ with this horrible disease ever again.
I would like to conclude with one last message. Women need to know that period pain IS NOT normal and that early detection and early intervention and treatment is the key to treating any disease properly. The earlier a woman is investigated and the disease is detected and managed properly, the better her future health and fertility outcomes are.
Please do not think that teenage girls are too young to have endometriosis. Early intervention and early treatment and management of this disease is crucial.
Lets end the silence about this horrible disease. Please support Endometriosis Awareness and support anyone bringing awareness and education about this disease that so many women now have.
If you would like to book in a consultation with me, please call my friendly staff, or using the automated emails system on the website. Let me hold your hand and care for you and assist you in every step of the way to better health and a better way to live daily.
Regards
Andrew Orr
-Women’s and Men’s Health Advocate
“Leaving no Stone Unturned”
“Period Pain IS NOT normal”