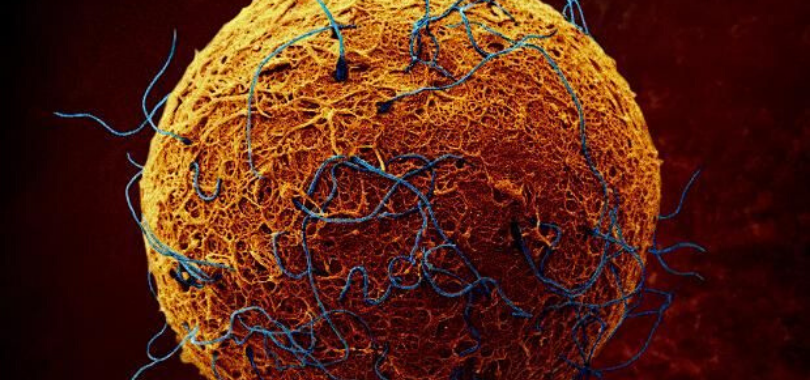
Research has now shown that sex around the time of embryo transfer increases the likelihood of successful early embryo implantation and development.
Intercourse during an IVF cycle has the potential to improve pregnancy rates and there is adequate research to now back this up. We know that in animal studies, exposure to semen is reported to promote embryo development and implantation.
Intercourse may assist implantation
This is actually good news for humans as well as it shows that intercourse may act to assist implantation. Animal studies reveal that exposure to seminal plasma, the fluid component of the ejaculate, is particularly important for achieving normal embryo development and implantation. Animals that become pregnant through artificial insemination or embryo transfer without being exposed to seminal plasma have substantially lower rates of implantation than those exposed to seminal plasma (Pang et al., 1979; Queen et al., 1981; O et al., 1988; Flowers and Esbenshade, 1993), while rodents inseminated with spermatozoa prior to blastocyst transfer also have a higher rate of implantation compared with those not exposed to spermatozoa (Carp et al., 1984).
Intercourse may influence pregnancy success rates
A multicentre prospective randomised controlled trial was conducted through IVF centred around the world, including Australia. The study was conducted to determine if intercourse around the time of embryo transfer, or just before and embryo transfer in an IVF cycle, actually has the potential to have any influence on pregnancy success rates.
Participants in Australian IVF clinics underwent frozen embryo transfer (FET) and participants in Spain IVF clinics did fresh embryo transfer. Participants were randomised to either have intercourse, or to abstain from intercourse around the time of embryo transfer.
The study showed that there was no significant difference in the pregnancy rates between those couples that abstained and those that had intercourse. However, the portion of transferred embryos that made it to 6-8 weeks gestation was significantly higher in the women exposed to semen compared to those who abstained.
This landmark multi-centre international study showed that women who had sex around the time of embryo transfer, and who were exposed to semen around the time of embryo transfer, had increased likelihood of successful early embryo implantation and development.
Couples need to be having more sex during IVF cycles
One of the things that I always promote as part of my fertility program, is that regular sex is so important for our fertility patients, on many levels. Sometimes the obvious eludes some people though.
One of the things we see quite regularly is that couples doing Assisted Reproduction (ART) are abstaining from sex fearing it will affect their chances of conceiving. Actually the opposite is true. By not having sex during ART cycles (IUI, IVF etc) you are affecting your chances of conception.
I have spoken about the importance of sex and orgasm assisting implantation in other posts and there is so much medical research to back this up. This is seen in the research I have talked about above.
Let’s be real and look at the facts
Let ask the question “If you were trying naturally, would you stop having sex for fear that conception has taken place?”
Then why would you stop having sex around an ART cycle?
Let’s face the facts, implantation takes place in the uterus, and not the vagina, and no man is that well endowed to even penetrate the cervix, so…. Let’s get a grip here
The question to ask is “What does an embryo feed off and need to successfully implant?”
The answer is blood!
Think of a tick borrowing into skin to feed off its host.
How do you get blood flow into the uterine lining?
The answer is that sex and climax stimulate blood flow to the lining to assist implantation and also prepare the lining for implantation. Nature has given us all the tools for healthy conception to take place, and yet many of us just aren’t using them.
Sex is more than just and egg and a sperm
Don’t forget that regular sex during this time not only helps assist implantation, but it also helps with the bonding process and physical connection process during this stressful time. Many couples split up because of losing this connection during the ART process and sex is a way of keeping that physical and emotional connection. Sex also tells your body you are also preparing to conceive on another level too.
For those doing IVF etc, next time you are doing an ART cycle maybe it is time to start doing things the way nature intended to give you that boost you so desperately are needing. Go get busy people
Final Word
If you are struggling to fall pregnant, or need advice with preconception care, please give my friendly staff a call and find out how my fertility program, which has helped over 12,500 babies into the world, may be able to assist you too.
Regards
Andrew Orr
– No Stone Left Unturned
-Master of Reproductive Medicine
-Master of Women’s Health Medicine
-The International Fertility Experts
References:
- http://humre.oxfordjournals.org/content/15/12/2653.short…
- Bellinge, B.S., Copeland, C.M., Thomas, T.D. et al. (1986) The influence of patient insemination on the implantation rate in an in vitro fertilization and embryo transfer program. Fertil. Steril. , 46, 252–256.
- Carp, H.J.A., Serr, D.M., Mashiach, S. et al. (1984) Influence of insemination on the implantation of transfered rat blastocysts. Gynecol. Obstet. Invest. , 18, 194–198.
- Coulam, C.B. and Stern, J.J. (1995) Effect of seminal plasma on implantation rates. Early Pregnancy , 1, 33–36.
- Fishel, S., Webster, J., Jackson, P. and Faratian, B. (1989) Evaluation of high vaginal insemination at oocyte recovery in patients undergoing in vitro fertilization. Fertil. Steril. , 51, 135–138.
- Franchin, R., Harmas, A., Benaoudia, F. et al. (1998a) Microbial flora of the cervix assessed at the time of embryo transfer adversely affects in vitro fertilization outcome. Fertil. Steril. , 70, 866–870.
- Franchin, R., Righini, C., Olivennes, F. et al. (1998b) Uterine contractions at the time of embryo transfer alter pregnancy rates after in-vitro fertilization. Hum. Reprod. , 13, 1968–1974.
- Marconi, G., Auge, L., Oses, R. et al. (1989) Does sexual intercourse improve pregnancy rates in gamete intrafallopian transfer? Fertil. Steril. , 51, 357–359.
- Pang, S.F., Chow, P.H. and Wong, T.M. (1979) The role of the seminal vesicles, coagulating glands and prostate glands on the fertility and fecundity of mice. J. Reprod. Fertil. , 56, 129–132.
- Qasim, S.M., Trias, A., Karacan, M. et al. (1996) Does the absence or presence of seminal fluid matter in patients undergoing ovulation induction with intrauterine insemination? Hum. Reprod. , 11, 1008–1010.