Vaginal bleeding between periods can be common and is not generally a cause for concern. Most of the time women will get just very light pink coloured watery flow, or just some spotting.
There can be many reasons why a woman would be getting bleeding between periods, which includes hormonal changes, injury, or an underlying gynaecological, or health condition.
While bleeding between your periods may not be cause for concern, on one level, the ideal situation is to not have any form of bleeding at all and if you do get bleeding between your cycle, it is a good idea to have this investigated, just to be on the safe side.
What a proper menstrual cycle should be like
I have done quite a few posts on what a proper menstrual cycle should be like, but I will go over this again just briefly
A proper menstrual cycle should be between 26-32 days in length and really only have about 3-5 days flow. Any longer than this can be too long and put a woman at risk of being low in iron, especially if this happens all the time.
The blood flow should be a nice red consistency, no clots, with no stopping and starting, and women shouldn’t have too many digestive disruptions, and really, a woman should not be getting pain with her cycle.
A little bit of distention and knowing the period is coming is fine, but there should not be pain at all. If you have to reach for the pain killers and the heat pack, or are doubled up in pain, this is not normal and you need to get this checked out.
What are the causes of bleeding between periods?
As mentioned before, there can be a variety of reasons for breakthrough bleeding, some of which are no cause for concern at all. Some however do need to be investigated.
Below are some of reasons for bleeding between periods:
Ovulation
When an egg is released from the ovary, it does create a tiny wound, through which the egg will then travel through the tubes and prepare to make its way to be fertilised, or then shed with the menstrual flow. At ovulation, this tiny wound can also create a tiny amount of bleeding, which can be seen as spotting during the ovulatory phase of a woman’s cycle.
Implantation bleeding
When an embryo implants into the uterine lining and begins to grow, many women experience spotting around this time. This is called implantation bleeding. They may also experience some slight cramping at the same time and all of this is quite normal. Some women may then experience some lighter bleeding as the embryo grows further. They usually get some light spotting, which can be a light pink, or a brown colour. Sometimes it can be more like fresh blood. While this is normal, it is a good idea to get this checked out just to be on the safe side and to also put the pregnant mothers mind as ease too.
Miscarriage
Bleeding between menstrual periods can be an early sign of a miscarriage. Many women may not even know they are pregnant and may be completely unaware they are having a miscarriage. While it is generally thought that once a woman reaches twelve weeks gestation everything is generally going to be ok, miscarriages can occur at any time during pregnancy.
Termination
After having a termination women can bleed for some time after the procedure, or taking the medication to start the abortion process. If bleeding continues and is very heavy, women need to seek medical advice.
Polyps
Polyps are small growths that can develop in the uterus or on the cervix. They are often a cause for unexplained bleeding between the cycles. Polyps do need to be removed as they can prevent implantation happening and they can also turn cancerous if left behind. Polyps are a very common cause of bleeding between periods.
Fibroids
Fibroids, or myomas (also known as leiomyomas, or fibromyomas) are growths, or benign (non-cancerous) tumours that form in the muscle of the uterus. Up to 40% of women over the age of 40 years have fibroids and as many as 3 out of 4 women develop fibroids in their lifetime.
Fibroids can cause heavy bleeding, extended bleed and painful periods. They can also cause infertility, miscarriage and premature labour. In many women, they will not cause any problems at all. Fibroids are a very common cause of bleeding between the cycles.
Polycystic Ovarian syndrome (PCOS)
Polycystic Ovarian Syndrome (PCOS) is a very common condition that can cause irregular periods, absent periods, and can also cause bleeding between periods. PCOS can also cause other issues such as acne, weight gain, infertility and hormonal and emotional disturbances.
Endometriosis or Adenomyosis
One in ten women are diagnosed with endometriosis and many more do not even know that they have it. Endometriosis and Adenomyosis are very closely related, with endometriosis usually being more superficial disease and not confined to the uterus, and adenomyosis being deep within the uterine tissue. Chronic conditions such as endometriosis and adenomyosis, can cause bleeding or spotting between periods. These conditions may also cause heavy or painful menstrual periods and cramps between periods. Adenomyosis will usually cause more bleeding symptoms along with pain etc.
Sexually transmitted infections (STIs)
Some sexually transmitted infections (STIs) can cause pain, vaginal bleeding and spotting. If you do suspect you may have a STI, you need to see your doctor for investigation and treatment.
Injury to the vaginal wall
During sexual intercourse the tissue of the vagina can be damaged and this can then cause bleeding. If the vagina is too dry, lack of arousal, and not lubricated enough this is more likely to happen. It can also happen if there is atrophy in the vaginal tissue as well. This is called atrophic vaginitis. This is more likely to be seen when a woman is going into menopause, or undergoing cancer treatments, or has diabetes.
Menopause or perimenopause
The menopausal stage of life and especially the perimenopause stage, can be a cause of irregular menses and irregular bleeding. It can also cause spotting, or heavy bleeding too. Perimenopause is the period leading up to menopause. This stage of a woman’s life can last for up to 10 years as hormone levels in the body change and can be unstable.
Hormonal contraceptives
Hormonal contraceptives are a common cause of bleeding between periods. They can also cause irregular bleeding and this can be quite usual in the first 3 months of using the contraceptive. If a woman misses takin her oral contraceptive, it can also cause irregular bleeding, or a withdrawal bleed. Intrauterine Devices (IUD’s) like the Mirena, will often cause irregular periods and irregular bleeding in the first 3 months after it have been inserted. If bleeding lasts for longer than 3 months on any contraceptive, it is a good idea to seek medical advice and get investigated and managed properly.
Emergency contraception
The morning after pill, or emergency contraceptives, may also cause bleeding. If bleeding persists, you should seek medical advice.
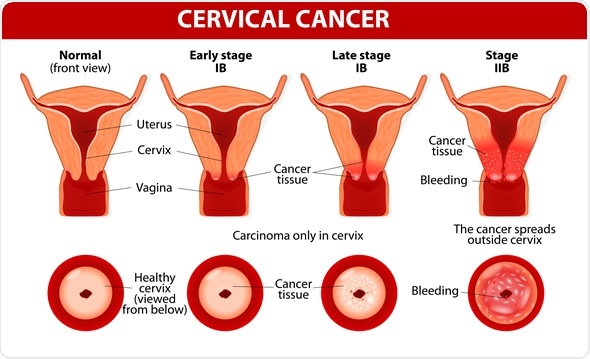
Certain cancers
Vaginal bleeding between periods can also be a sign of gynaecological cancers in women. Most bleeding that women get is not serious, but it still needs to be checked. Cervical cancer can affect women of any age. Bleeding between the cycle, or after intercourse, and pain after intercourse, or unpleasant smelling discharge can be symptoms of cervical cancer and these all need to be checked by your doctor, or gynaecologist.
Uterine cancer tends to occur in women over 50 year of age. One of the early symptoms of uterine cancer can be vaginal bleeding. Uterine cancer mostly affects women are in the menopause and no longer have periods, so this is why any bleeding after menopause needs to be investigate and seen as not being normal.
Stress
Yes, stress can cause abnormal bleeding and also interfere with a woman’s cycle. Increased levels of stress can interfere with hormones and this can lead to bleeding, irregular cycles, or pain with cycles too.
When to see a doctor
If vaginal bleeding between periods is heavy, persistent, or unusual then a woman should go and see a specialist, or a gynaecologist, who is a specialist in this area of medicine. As mentioned previously, while some causes of bleeding are not serious, some are and need to be properly investigated and properly managed medically.
Treatment and prevention
All women should keep a record of their menstrual cycle and when the period starts and how long it lasts for. Any abnormal bleeding should be recorded so that you can show your healthcare specialist if need be. Any abnormal bleeding should be investigated and the treatment will depend on what the underlying cause is.
Women should try and see their healthcare specialist for regular pap smears and regular check-ups for gynaecological health.
If women are getting small tears and bleeding caused from dryness in the vagina, then there are water based lubricants that can be used to help with lubrication and to moisturise the surrounding tissue.
There is no cure for gynaecological and reproductive issues such Endometriosis, but these disease states can be treated and managed to give women a normal life.
Proper treatment of these issues needs a “Team”, or multimodality approach using medical options, surgical interventions, pelvic floor specialists, complementary therapies, hormone therapies, and diet and lifestyle changes. It is about using what works for the individual and not a blanket one treatment fits all approach.
Last but not least, all women should know that period pain is not normal and that irregular bleeding really isn’t normal either. While most causes of bleeding are not life threatening, they still need to be investigated and checked out properly. Never ever put off seeing a medical specialist if you have abnormal bleeding.
If you would like to book in a consultation with me and find out how I can assist you with women’s health conditions, please give my friendly staff a call and they will be able to assist you.
Regards
Andrew Orr
-No Stone Left Unturned
-Women’s and Men’s Health Advocate