Why does the body need Iodine?
Iodine is a water soluble mineral that is needed in our diet to ensure that the thyroid works properly.The thyroid gland uses iodine to make thyroid hormones.
Thyroid hormones play an important role in a wide range of bodily functions, including metabolism, bone growth, immune response, and development of brain and the central nervous system (CNS).
Iodine helps convert thyroid stimulating hormone (TSH) to triiodothyronine (T3) and thyroxine (T4). This conversion is important for the thyroid to function properly.
Iodine is essential for brain development, bone health, healing, immune response, energy, metabolism and the development of the central nervous system. We also now know that we need iodine to help with pregnancy and fertility. Iodine deficiency during pregnancy and early childhood can also lead to developmental problems.
An iodine imbalance can lead to an overactive, or under-active thyroid.
Being deficient in iodine limits the ability of the thyroid gland to make hormones, causing hypothyroidism. Hypothyroidism happens when a person’s thyroid does not produce enough thyroid hormones. Hypothyroidism can cause symptoms of fatigue, depression, forgetfulness, hair weakness, hair loss, dry skin, weight gain, cold intolerance and constipation.
Signs of iodine deficiency
According to new research published last year, it was estimated that about a third of people are deficient in iodine. Here are some of the common signs that could suggest that a person may have an iodine deficiency.
1.Weight gain
One of the most noticeable signs of an iodine deficiency is unexpected weight gain.
When a person has a healthy metabolism, they burn calories to give them their energy. Hypothyroidism, or a lack of thyroid hormones, can slow down a person’s metabolism and this can then lead to weight gain. It is important to remember that weight gain is not always a sign of an iodine deficiency. It may only be a symptom when weight gain cannot otherwise be explained. Eating foods that are highly refined and high in sugars are probably the most common form of increase weight.
2.Feeling weak & lethargic
When a person has an iodine deficiency, they may feel weak and lethargic. Hypothyroidism can slow down a person’s metabolic rate and then they burn fewer calories for energy. When they have less energy, the muscles do not work as efficiently and then the person would feel weak. But, feeling weak may also be from other factors such as lack of sleep, lack of essential nutrients, lack of food intake and nutrient deficiencies. This may also be a sign of other health issues and needs to be investigated if it goes on too long.
3.Feeling tired
Unexplained tiredness may be a symptom of iodine deficiency. When a person is iodine deficient their metabolic rate may drop and this could cause them to feel tired. But, feeling tired does not always mean a person is iodine deficient. As mentioned before, if a person is not getting enough rest, it is natural for them to feel tired. Feeling tried could also be a sign of iron deficiency, or other health issues, but, if tiredness is unexplained, it may be a symptom of an iodine deficiency.
4.Hair Loss
Hair loss is another possible sign that a person might have an iodine deficiency.
Thyroid hormones support the renewal of hair follicles and when someone has hypothyroidism, a shortage of thyroid hormones means the hair follicles stop being renewed. It is natural for hair to fall out, but it is normally renewed. But, while hair loss can be a sign of iodine deficiency, it can also be caused by other hormonal issues as well as stress. Stress is one of the most common causes of hair loss.
5.Drying skin
Having dry, flaky skin could be a sign of hypothyroidism, and can be the result of iodine deficiency. Thyroid hormones help with the renewal of new skin cells. A lack of these hormones and a deficiency of iodine, may cause dead skin cells to build up, sometimes resulting in dry, flaky skin. While dry skin can be caused by iodine deficiency, it can also be caused from other factors such as lack of hydration, lack of essential oils and other health conditions
6.Feeling cold
Iodine deficiency causes a lack of thyroid hormones, which can then affect a person’s metabolic rate to slow down. As their metabolism slows down, a person produces less energy to give the body warmth. A lack of energy and lack of body heat will mean a person is more likely to feel the cold. But, feeling cold isn’t always a sign of iodine deficiency and can be a sign of lack of circulation and other health issues.
7.Having a slow heart rate
Having an iodine deficiency may make a person’s heart beat more slowly.
When a person’s heart rate slows down, they may feel a bit dizzy, nauseas, or sick. It may also make them feel a bit faint. But feeling this way may also be a sign of other health issues, or it could also be a sign of a virus, or issue with someone’s cardiovascular system and needs to be checked out.
8.Learning or memory problems
Thyroid hormones are important for brain development and Iodine deficiency may cause a lack of these hormones, resulting in problems with memory and learning. Studies have shown that people, who are deficient in iodine and have lower level of thyroid hormone, may have parts of their brain being smaller and this then affects their memory. But while this may be the case, learning and memory problems could be caused from other health issues and need to be checked out properly
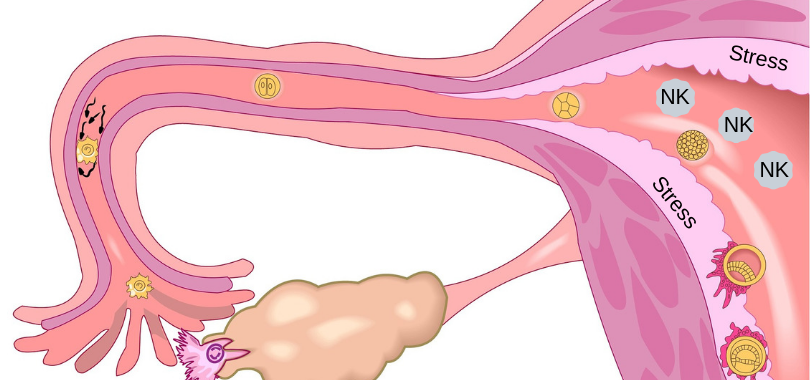
9.Pregnancy complications
Iodine deficiency may cause issues during pregnancy for the developing baby and it can be harder to get enough iodine during pregnancy. Not only does a women need iodine for herself, but she needs it for the growing baby inside of her as well.
Thyroid hormones are necessary for the healthy development of a baby before it is born. A lack of iodine and thyroid hormones may prevent the baby’s brain developing properly. It may also affect their immune system and affect their growth. If a pregnant woman’s body is too low in iodine it could cause her baby to be stillborn.
10.Heavy or irregular periods
Deficiency in iodine can lead to low thyroid hormone levels, which can then affect the levels of hormones that regulate a woman’s periods. Iodine deficiency can lead to periods that are heavier than usual, or the periods that are more or less often than usual. While, iodine deficient could cause abnormal abnormalities in a woman’s menstrual cycle, irregular or heavy periods are usually a sign of gynaecological conditions that needs to be evaluated by a specialist.
11.Swollen neck and goitres
If a person is deficient in iodine, the thyroid gland can become enlarged and this can then make the neck become swollen. This can lead to a condition called goitre. Abnormalities with the thyroid gland and hormones can also cause growths called nodules.
When the thyroid does not have enough iodine, it will try to absorb more from the blood and this then causes the thyroid to become enlarged, making the neck appear swollen.
Complications and diagnosis.
An iodine deficiency may happen when a person does not consume enough foods that are rich in iodine, or have adequate supplementation. This deficiency is more likely to affect pregnant women who need a higher intake of iodine.
Pregnant women and their babies experience the most serious complications of iodine deficiency. In the worst cases, it can lead to babies being stillborn or born with mental issues due to stunted brain development.
If you think you may be deficient in iodine you can go to your doctor and they can organise proper testing for you. The most effective way to diagnose iodine deficiency is via a urine test.
If you have a family history of thyroid issue, or are to conceive, or are pregnant, you should be supplementing with iodine based multivitamins or individual supplements. A person needs to consume 150 micrograms (mcg) of iodine each day to maintain a healthy level for their body. You should also be looking at eating iodine rich foods daily as well.
The following are good sources of iodine:
- Seaweed
- Cod, tuna, salmon and white fish
- Plain Yogurt, Cheese and Milk
- Iodized salt
- Shell fish and oysters
- Eggs
- Dried prunes
Regard
Andrew Orr
-No Stone Left Unturned
-Women’s and Men’s Health Advocate