In the last couple of weeks I have been talking about the serious complications of people not having their health managed properly. It seems to be a big issue and with my latest post, the issue of unmanaged, or undiagnosed low iron is also becoming a very serious issue indeed. So for this post I will be talking about the serious health complications of low iron.
Two thirds of body iron is present in circulating red blood cells known as haemoglobin. Each gram of haemoglobin contains about 4gms of iron and each ml of blood lost from the body results in a loss of about half a milligram of iron.
Bleeding is the most common cause of iron deficiency. This could be from either a diagnosed, or undiagnosed gynaecological issues (endometriosis, adenomyosis, fibroids, polyps, other) or it could be from a parasite infection. It could also be from bleeding as part of a gastrointestinal issue, or part of inflammatory bowel diseases (IBS, Crohn’s Coeliac disease).
There could be other reasons for blood loss in the body, or reduction of iron and many of these conditions, and the conditions above, can go unrecognised and then cause iron deficiency anaemia. Some of these issues can be very serious, or even fatal.
Excessive menstrual losses are often overlooked with many women. This is something that should not happen and should be part of the questioning with any low iron status. The problem is, unless the menstrual flow changes, patients typically do not seek medical attention for heavy menstrual bleeding. Sometimes when a healthcare practitioner asks, these patients generally report that their menses are normal. It may be normal to them, but we need to educate women that heavy blood loss is not normal and can lead to anaemia.
Because of the marked differences among women with regard to menstrual blood loss (10-250 mL per menses), patients meed to be asked about their menstrual history and about a specific history of bleeding, blood flow, abnormal bleeding in between cycles, clots, cramps, and the use of multiple tampons and pads. These are very important questions to ask and sadly many women are not being asked these questions, or having further questioning about their menstrual, or overall health, including dietary intake etc.
What is iron deficiency anemia?
Anaemia occurs when you have a decreased level of haemoglobin in your red blood cells (RBCs). Haemoglobin is the protein in your red blood cells that is responsible for carrying oxygen to your tissues.
Iron deficiency anaemia is the most common type of anaemia that women present with, and it occurs when your body doesn’t have enough iron. Your body needs iron to make haemoglobin. When there isn’t enough iron in your blood stream, the rest of your body can’t get the amount of oxygen it needs. Today in a recent post I talked about iron being like trucks, or the transporters of oxygen around the body.
While iron deficiency may be common, many people don’t know they have iron deficiency anemia. It’s possible to experience the symptoms for years without ever having it diagnosed, or the cause of the iron deficiency diagnosed either. It is a very serious issue that needs some serious attention.
In women of childbearing age, the most common cause of iron deficiency anemia is a loss of iron in the blood due to heavy menstruation or pregnancy. A poor diet or certain intestinal diseases that affect how the body absorbs iron can also cause iron deficiency anemia. Women who adopt a vegan diet will also be prone to being iron deficient and vitamin B12 deficient.
Disruption to the microbiome and leaky gut syndrome can also cause iron deficient anaemia too.
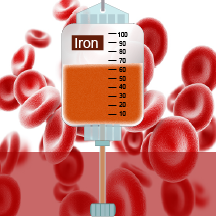
One of the best ways to treat the condition is through iron infusion, and also with iron supplements, or changes to diet. We also need to make sure the cause of the iron deficiency is addressed as well.
Symptoms of iron deficiency anaemia
The symptoms of iron deficiency anaemia can be mild at first, and some people may not even notice them. Many people are completely unaware that they may be low in iron, or are actually iron deficient.
The symptoms of moderate to severe iron deficiency anaemia include:
- general fatigue
- weakness
- pale skin
- Bruising easy
- shortness of breath
- Palpitations
- dizziness
- Strange cravings to eat items that aren’t food, such as dirt, ice, or clay
- Tingling or crawling feeling in the legs
- Tongue swelling or soreness
- Cold hands and feet
- Tachycardia
- Brittle nails
- Headaches and migraines
- Sore joints
- Brain fog and lack of concentration.
The serious complications of unmanaged iron deficiency.
Undiagnosed, or unmanaged iron-deficiency may cause the following severe complications:
- Heart problems.If you do not have enough hemoglobin-carrying red blood cells, your heart has to work harder to move oxygen-rich blood through your body. When your heart has to work harder, this can lead to several conditions: irregular heartbeats called arrhythmias, a heart murmur, an enlarged heart, or even heart failure.
Severe anemia due to any cause may produce hypoxemia and enhance the occurrence of coronary insufficiency and myocardial ischemia. - Increased risk of infections- Research has shown that iron deficiency anaemia can affect your immune system (the body’s natural defence system), making you more susceptible to illness and infection.
- Motor or cognitivedevelopment delays- This mainly occurs in children. Children deficient in iron may exhibit behavioral disturbances.
- Behaviour issues and mood disorders- Behavioral disturbances may manifest as an attention deficit disorder, or mood disorder such as : Depression Unipolar depressive disorder, Bipolar disorder, Anxiety disorder, Autism spectrum disorder, Attention-deficit/hyperactivity disorder, Tic disorder, Delayed development and other some other psychiatric issues.
- Pregnancy complications- Iron deficiency can lead to preterm delivery or giving birth to a baby with low birth weight.
The neurologic damage to an iron-deficient foetus results in permanent neurologic injury and typically does not resolve on its own, or by supplementation. - Chronic Health Conditions worsened- In people with chronic conditions, iron-deficiency anaemia can make their condition worse or result in treatments not working as well.
- Dysphagia (Difficulty swallowing)- This may occur with foods due to abnormal muscle and nerve control. This could result in choking. It can also lead to throat cancers.
- Atrophic gastritis – This occurs in iron deficiency with progressive loss of acid secretion, and causes inflammation of the gastric mucosa with loss of the gastric glandular cells and replacement by intestinal-type epithelium, and fibrous tissue
- Tiredness- As iron deficiency anaemia can leave you tired and lethargic (lacking in energy), you may be less productive and active at work. Your ability to stay awake and focus can be reduced, and you may not feel able to exercise regularly.
- Fainting– Low iron can cause fainting and this could be dangerous in many situations, especially at work places, or working on machinery, or driving a car.
- Cold Intolerance– Cold intolerance develops in one fifth of patients with chronic iron deficiency anaemia and is manifested by neurologic pain, vasomotor disturbances, or numbness and tingling.
- Issues with Brain and Optic Nerve– Rarely, severe iron deficiency anaemia is associated with papilledema (optic disc swelling), increased intracranial pressure, and the clinical picture of pseudotumor cerebri. These manifestations are all corrected with iron therapy.
- Migraines– Research has now shown that there are certain types of migraines caused by iron deficiency
- Death – Caused by some of the issues mentioned above
The importance of proper management
Hopefully now everyone can see why iron is so important and that people with iron deficiency need to see their healthcare practitioner for proper help and proper management . Iron deficiency anemia isn’t something to self-diagnose or treat. It needs to be diagnosed, treated and managed properly. In many cases an iron infusion is the best and quickest way to get iron levels back up. Have a read of my post about iron infusions. Click here
Iron infusions are the quickest way of getting iron levels back up
In the case of low, or severely low iron, supplements just are not enough. They take too long to get levels up and the damage to your body in waiting too long can also be serious. Always see your healthcare practitioner, or specialist, for a diagnosis rather than trying to manage low iron on your own, or just taking iron supplements on your own. Overloading the body with too much iron can be dangerous too, because excess iron accumulation can damage your liver and cause other complications.
Final Word
This is why everyone needs to be managed by a properly trained healthcare professional with any health issue, especially low iron. If your practitioner is not able to assist you, please make sure you get a second or third opinion. Some practitioners may not be well versed in the serious complications of low iron, or know much about iron infusions etc.
If you do need help with managing the symptoms of low iron, you can call my friendly staff and find out how I can assist you. For more information please call +61 07 38328369 or email info@drandreworr.com.au
Regards
Andrew Orr
-No Stone Left Unturned
-Master of Women’s Health Medicince
-Master of Reproductive Medicine
-Women’s and Men’s Health Advocate